As the medical care industry faces unprecedented challenges due to the Covid-19 pandemic, medical billing management has been exposed to its own set of dilemmas. As infections across the nation grow with the Covid-19 outbreak, the health and safety of patients lie as the top priority in medical care. The covid-19 pandemic has also caused a massive outbreak of unemployment and financial insecurities, which has created a direct impact on healthcare payment. Covid-19’s impact has made its way across the entire medical billing system and healthcare payment system. Care-givers have to now deeply analyze the best options for enhancing the patient experience.
Medical billing in Covid-19 is faced with the challenge of adjusting to covid-19 billing requirements, avoiding surprise medical billing, and enhancing the medical billing process through healthcare cloud solutions. Medical billing policy has to adapt to the present times and remain geared to address the economic losses faced by healthcare organizations. This is caused due to the sudden decline in outpatient and non-urgent treatment procedures.
Statistics:
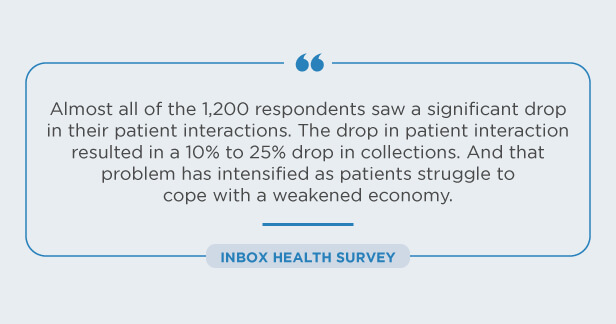
“According to an Inbox Health Survey of 1200 medical billers, 21% of the respondents forecast that 10-25% of their practices may close their practice within the next six months. Another 18% of respondents said they expect that 25-50% of their practices will shut their doors. Congress has provided over $100 billion to help medical practices, hospitals, doctors, and other healthcare professionals in the Public Health and Social Services Emergency Fund through the Coronavirus Assistance, Relief and Economic Stability (Treatment) Act, or the Provider Relief Package.”
Medical Billing Strategies To Maintain Scalability:

As medical billing in covid-19 continues to be strained, healthcare organizations need to adapt to custom healthcare solutions to manage healthcare revenue cycle management. As billing codes evolve and healthcare payment systems cope with the changes, we have listed out some strategies for medical billers to stay ahead in the game:
Adaptation: Whether it’s covid-19 medical bills or general medical bills, billing automation needs to be synced with the evolving rules and regulations for medical billing compliance. Deploying agile clinical coding solutions can be a step in the right direction.
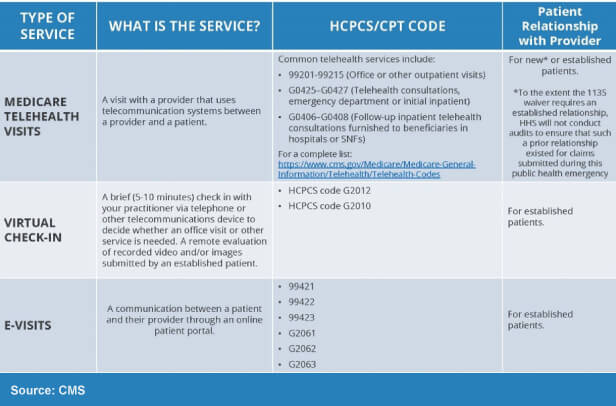
Telehealth: Telehealth billing and telehealth coding are probably the most important tools that have emerged for medical billing in covid-19. Healthcare billing must factor in insurance verification in the billing process, documentation needs, and approvals through healthcare automation.
Remote Payment Systems: Tighter controls over the remote medical billing process will minimize cash flow. As the covid-19 pandemic causes economic distress, this process of medical billing best practices can be enabled through case management software.
Medicare Risk Score: The health risk score needs to be keenly examined to avoid overall losses. EMR systems can be used to account for changes in co-pays and deductibles towards patient-friendly billing. This will consequently minimize medical billing denials and actions.
Patient Experience: Medical billing issues can be resolved by recording changes in referrals, optimizing patient billing, and health insurance eligibility verification through an intelligent hospital management system. Actions such as these will increase patient experience through a boost in trust and confidence.
Medical Billing Codes: To address the issue of denial management in medical billing, medical bills need to adhere to the evolving covid-19 CPT codes. ICD-10 codes solutions can assist in this domain to a large extent. Coronavirus medical bill operations have constantly been evolving, and healthcare organizations have to keep up.
Billing Management: Apart from billing compliance, another important factor is to consider the changing scenario of medical billing in covid-19. Due to increased unemployment, more and more people will be uninsured as time goes by. Billing reconciliation will then be more dependent on self-pay than on Medicare payments.
Reducing Denied Claims: Medical claims management solutions can go a long way towards denial management in healthcare. This is accomplished through error identification and rectification before the claims are rejected. Healthcare organizations will find themselves at a risk advantage for medical billing in covid-19. Automated healthcare provider solutions further increase the probability of customizations and reduced errors, with an increased bottom line.
New CPT Codes and Other Updates:
New Guidelines:
Medical billing in covid-19 has witnessed a surge of changes in medical billing codes. The precision and accuracy of insurance verification and Covid CPT codes are of utmost importance toward the flow of revenue. As healthcare organizations are challenged with increasing pressure for diagnosis, treatments, and follow-up care, Covid billing is another massive hurdle that needs to be surpassed. New coding details and guidelines have to be adhered to with utmost efficiency for maximum profit.
Updated Codes:
Integrated healthcare solutions need to be agile enough to account for Covid Medicare payments through ICD-10 CM coding. These Medicare CPT codes have been released and updated, along with the Cares Act Provider Relief Fund. Medical billing solutions also need to factor in the Covid risk score of patients. From testing to diagnosis and treatment of covid-19 patients, medical billing in covid-19 has seen the emergence of new codes like never before.
Denial Management:
As financial uncertainty continues to reign, denial management of codes through accurate payment posting in medical billing requires extra care. Providers must adopt additional mechanisms to ensure minimal denials through remittance software solutions for Medicare Covid payments. Medicare payments for covid-19 require deep analysis toward accuracy to ensure adherence to the new codes. Specialists can be deployed to take on this task. Finally, an important factor toward gaining patient trust is to steer clear of surprise billing.
What is Surprise Billing:
Surprise billing is a term that literally defines an outrageous, unexpected bill. Even when a patient has done enough research, picked optimum health plans, and been regular with their premiums – they can still be at risk of surprise billing. Surprise medical billing occurs when a patient goes to an in-network facility but receives care from an out-of-network doctor. This loophole in the U.S. healthcare system has caused enormous distress to patients. It would be prudent for the healthcare organization to inform the patient about the costs involved with surprise billing before they receive the care.
Ways in Which Medical Billing Systems Can Prevent Surprise Billing:
Healthcare billing solutions, such as medical credentialing and medical records management, can protect patients from surprise billing. This will, in turn, enhance patient satisfaction and improve the bottom line of the healthcare organization. Even with medical billing in Covid-19, coronavirus medical bills and Medicare covid-19 payments can be adapted within this protective shield through the analysis of patient advantage scores. As several states have recognized this problem, they are addressing it through modified Covid-19 payment strategies.
Examples From Around the Nation:

“For example, Becker’s ASC Review noted that “Connecticut adopted a policy to ensure patients are protected from incurring surprise medical bills for treatments provided during the pandemic.” For patients in Connecticut who were treated by health care professionals while “out of network,” the encounters have to be considered as in-network due to the state of emergency of the growing global pandemic of the novel coronavirus.”
“ASC Review also reported that 56% of Americans believe that their representatives must address the issue of surprise medical bills, based on figures from a 2019 tracking poll by the Kaiser Family Foundation. And currently, leaders from two congressional committees are working on legislation for upcoming pandemic stimulus bills, to ban surprise medical bills nationwide.”
Conclusion:
Medical billing in Covid-19 times is looking toward innovative strategies to surpass the challenges of revenue loss, among recession and unemployment. The healthcare industry has been faced with a plethora of hurdles and will need to adopt agile technologies and best practices to remain afloat. Robust medical billing practices are the need of the hour to address the losses in the revenue cycle from the financial impact on medical billing in Covid-19.
Sustaining the medical billing process through inpatient procedures seems like a distant possibility at this point. As healthcare strategies evolve and move towards telemedicine, medical billing needs to adhere to the evolving panorama. Urgent care procedures have to be streamlined toward the new normal, with all the necessary measures put in place and medical billing in Covid-19 is no exception. Sustaining the business may have never been this challenging, but there is light at the end of the tunnel.
Reassessing financial plans to mitigate the impact of the pandemic through telemedicine solutions will build patient confidence and experience, leading to a boost in medical billing in Covid-19, and ultimately, higher revenue. It is safe to say that almost 9 million beneficiaries have already partaken of telemedicine services, and that number is only poised to increase. As the game-changer in healthcare, telemedicine is the need of the hour, and medical billing has to adapt to the same. The benefits of telehealth solutions are far-reaching, and medical billing in Covid-19 stands to gain its maximum through this avenue.
Payer billing tactics and payer mix are entitled to change as well. High-deductible health plans have been replaced by self-pay methods to improve the billing scenario. A digitally-enabled healthcare billing platform is the need of the hour and will continue to be the same in the future. Not only will telehealth address ‘crisis’ situations, but it needs to be enabled toward providing regular care models. New reimbursement policies, accurate evolved coding, and adherence to new CPT codes are another important dimension in medical billing.
References:
https://1stproviderschoice.com/significant-impact-of-the-covid-19-pandemic-on-medical-billing/
https://www.adsc.com/blog/impact-covid-19-pandemic-medical-billing
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.