Blogs
Enhancing the Abilities of Healthcare SectorServices
Solutions
Services
Solutions
Revenue cycle management (RCM) in healthcare consists of all the activities at medical organizations surrounding the administration of finances and revenue. Healthcare revenue cycle management software is a technology solution streamlining healthcare operations like billing, claims, and payment processing. Custom-built RCM platforms enable healthcare organizations to consolidate their financial management activities and make strategic decisions to improve revenues. This applies to small practices with one or more physicians, medium-sized ambulatory care centers, and even large hospitals.
Healthcare RCM services ensure healthcare practices gain an optimal return on their investment. A full suite of healthcare revenue cycle software helps healthcare providers by streamlining healthcare RCM process. Revenue cycle healthcare needs constant monitoring to enhance reimbursement cycle and optimize patient-to-payment course.
Rather than healthcare RCM outsourcing, building your own customized healthcare revenue cycle management software proves beneficial. OSP has hands-on experience in building healthcare RCM software solutions that help in providing seamless revenue flow, enforce accurate policies, deploy time-sensitive bandwidth, facilitate compliance with regulations and reduce claim denials. Our solution for revenue cycle in healthcare can alleviate the labor-intensive manual tasks such as filing claims, working unpaid claims, exclusions, filing appeals, payment posting, secondary insurance claim filing, patient billing, etc.
As per the study by the American Medical Association (AMA), almost $15,000 per year is spent on investigating, reviewing and reworking the denied healthcare claims. Patient’s insurance eligibility issues are one of the most common reasons for claim denials. Insurance eligibility verification is the process of checking a patient’s health coverage and insurance eligibility to know the patient’s capacity to avail healthcare treatments and consultations.
Our healthcare RCM services are customized with advanced patient insurance eligibility verification module. It helps providers to track the insurance eligibility in real-time for all private health plans, Medicaid and Medicare. To streamline healthcare revenue cycle management, we can include claims scrubbing module to identify errors in CMS1500 submissions. With custom healthcare RCM, a payer rule engine in compliance with HIPAA and health plan guidelines is made possible. Our healthcare revenue cycle management services help to automatically verify procedure-specific coverage, perks, and all out-of-pocket costs.
RCM patient management software solutions are a collection of software systems that help to track the patient’s information medical diagnoses, prescriptions, interactions and encounters within healthcare organizations. We smartly integrate various patient management modules in healthcare RCM such as EHR/EMR, medical scheduling, practice management system (PMS), patient encounters and more.
OSP can build healthcare revenue cycle solutions that combine next-gen PMS systems that automate the routine processes such as patient flow management and helps healthcare providers to minimize their administrative expenses. A healthcare revenue cycle optimization can streamline all elements of a provider setting including recordkeeping, charting, medical appointment scheduling, billing, and claims processing functions. Our healthcare revenue cycle services simplify day-to-day operations with automated process management and timely patient care.
Medical billing is the system of submitting and following up on medical claims with healthcare payers to get reimbursed for treatments provided by a healthcare provider. OSP’ healthcare RCM services incorporate medical billing systems, developed with point-of-care care processing to support in-house billing process efficiently. The healthcare revenue cycle solutions can manage copays, deductibles, and coinsurance with smarter account reconciliation with patients via next-gen online payment portals.
Our medical billing services offer end-to-end healthcare revenue cycle optimization that automates follow-up requests for delayed as well as underpaid reimbursements. Our integrated healthcare revenue cycle management services can combine audit tracking software to archive every transaction in a simplified database. We eliminate revenue leakages by streamlining your entire healthcare revenue cycle workflow from eligibility verification, to check in, and co-pay collection to help you optimize revenue collection.
Medical coding is the process of translating the medical diagnosis, procedures, treatments, and equipment into ICD-10 codes to simplify the billing process. Our customized healthcare revenue cycle software can be integrated with EHR/EMR to pre-populate superbills with accurate ICD-10 and CPT codings following CMS.
The traditional manual medical coding process is labor-intensive, expensive, and prone to errors. We provide automated medical coding software solutions that are in line with ICD-10 and CPT codings. OSP’ healthcare revenue cycle management services include high-quality medical coding solutions for all medical specialties, subspecialties, and telehealth. Our tailored healthcare RCM software ensures minimum coding errors and claims denials with highly accurate and prompt medical coding services.
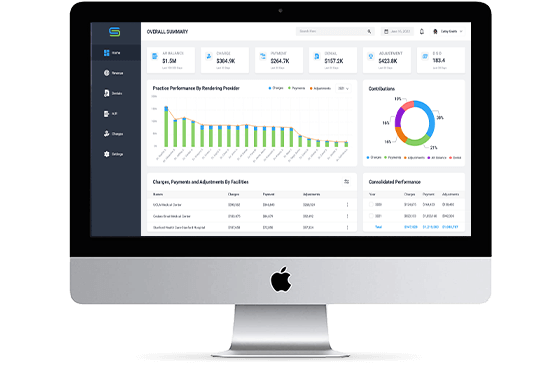
A revenue cycle for healthcare without advanced reporting module may have hidden problems that may grow worse with the time. Most healthcare revenue cycle management companies fail to focus on reporting that have long-term adverse effects on medical practice. OSP can build a made-to-order healthcare revenue cycle analytics that has custom reports, including financial data, management information and key performance metrics to see if your business is meeting benchmarks.
Our healthcare revenue cycle analysis solutions are capable of analyzing clinical and financial data from the data repositories, practice management systems, hospital information systems, medical billing systems and more. With in-depth healthcare revenue cycle analysis, you can find missed revenue opportunities, common coding errors, inadequate patient data capture, poor patient engagement and more. The healthcare revenue cycle analytics ensures intuitive data visualizations to understand the reports quickly.
One of the biggest advantages of using RCM software is the reduction in operating costs for providers. In the absence of such solutions, providers would need to hire a certain number of people to handle the billing and financial part of healthcare operations. But OSP can build tailored revenue cycle management software for consolidating these activities and enable a smaller staff to do what would otherwise have needed more people
Reimbursements from payers account for most of the revenues for providers. So, errors in claims that might result in denials or rejections can cost a provider precious revenue. But using revenue cycle management systems, we would build and digitize many workflows and automate them. As a result, the chances of denials and rejections from payers are reduced significantly, which means that healthcare providers can enjoy steady revenue cycles.
Revenue cycle software goes a long way in streamlining, optimizing, and simplifying the entire process of managing revenues in healthcare. This ultimately benefits the providers, payers, as well as patients themselves. When providers spend less time worrying about revenue management, they can devote more time to patients. Moreover, our healthcare revenue cycle software makes payments more convenient, further helping the patients. To sum it up, such platforms improve the overall experience for patients.
OSP's RCM application is a one-stop solution for all your billing and revenue cycle needs. Streamline your workflows, identify scopes of cash flow and reduce denials.
SIGN UP FOR DEMO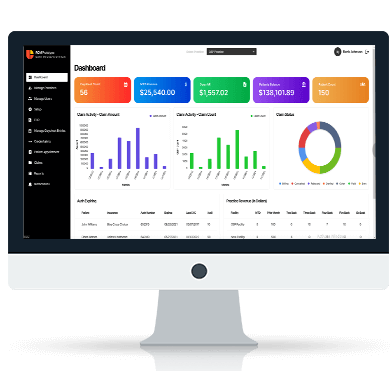



Revenue cycle management (RCM) in healthcare consists of all the processes in which medical services rendered to patients are billed and the payments collected. It begins with the patient’s appointment or clinical visit and ends when the provider, hospital, or clinic gets paid in full. The payment can come from the patients and insurance payers, depending on the type of insurance coverage plan of the patients.
Revenue cycle management (RCM) is how healthcare organizations to bill for their services. The process begins when the patients schedule their appointment and ends with the final payment made. It involves tracking all the services provided, transcribing them, translating them into standardized codes, and using these codes to fill out claims to be sent to payers. While most payments come from insurance payers, some also come from patients.
The revenue cycle management workflow comprises all the steps involved in billing and payment collection for medical services rendered to patients. They are –
The entire process of the healthcare revenue cycle can be categorized into three main phases –
Appointment Scheduling and Patient In-Take
Patients who schedule appointments fill out in-take forms before seeing a doctor. Subsequently, the staff verifies the patients’ health plans to ensure they are eligible for care services.
Charge Capture and Claims
Charge capture is when the clinical staff records all medical services. This is followed by transcribing the service into standardized codes to be filled out in claims and sent to payers. If there are some problems detected in the clams, the payer denies it or rejects depending upon the problem.
Payments Collections
The payers reimburse the providers for the medical services rendered to patients. The staff then posts the payments against the corresponding patient accounts to settle the claims. Remittance posting, followed by payment processing, is the last phase of the healthcare RCM cycle. In case of denials from payers, the provider will analyze the claim and the reason for the denial and take necessary steps to rectify the problem.
Healthcare in the United States is complicated. It involves an elaborate series of steps, from the patient’s clinical visit to the final payment. A dedicated process or software for revenue cycle management (RCM) will ensure that all the steps are carried out smoothly without any problems.
This ensures that the providers get paid on time without any delays. An efficient RCM system ensures that a medical organization can stay financially feasible and continue to serve patients.
The steps involved in revenue cycle management (RCM) include the following –
A robust process for managing revenue cycles ensures that providers can get paid on time without delays or hassles. This will enable them to remain financially feasible and continue caring for their patients.
Revenue cycle management (RCM) solutions are software platforms that enable providers or healthcare organizations to carry out billing operations. This software accelerates all the activities in the billing operations and automates manual, repetitive workflows. This increases the speed of operations and minimizes the chances of errors by limiting human involvement. As a result, RCM solutions boost billing operations’ overall productivity and efficiency, ensuring timely revenues for providers.
A revenue cycle management (RCM) platform is a software solution for carrying out all the billing operations at healthcare organizations. It replaces all the manual processes with digital ones, streamlining all the activities in the entire billing operation. Furthermore, this software also leverages automation to eliminate the need for people to carry out repetitive manual activities, thereby improving the speed and productivity of the entire billing process.
The four steps in revenue cycle management are as follows –
The revenue cycle management process begins even before the patient sees a doctor for consultation. It begins with the pre-registration of patients, followed by insurance verification.
Subsequently, the patient sees the doctor and receives the required care services, including a consultation or a consultation with prescriptions, tests, and so forth. This is followed by charge capture, where the staff record all the billable services rendered to the patients. This is then translated into medical codes, which are used to fill out claims to be submitted to payers.
The payer will reimburse the provider if the submitted claim is without errors. But in case of problems with the claim, the payer denies it, after which the provider needs to manage the denial to address the problems.