Patients go to doctors without much knowledge about their qualifications and certifications. Sometimes what meets the eye may be deceptive. Doctors may lack the certification required to render certain care services, which could pose a huge risk, besides going against the law. So, how do you check whether a physician has the required certifications and experience to perform their duties?- With the help of health care credentialing. Medical staff credentialing software in healthcare is a process that allows healthcare organizations to verify the education, training, and practice history of physicians.
There are three primary phases of credentialing process for medical staff: gathering information, verifying the data, and awarding the doctor with credentials. A medical credentialing software ensures that healthcare professionals have the necessary licenses, certifications, and skills to care for patients properly. Medical staff credentialing is also known as physician credentialing or doctor credentialing. According to the federal Centers for Medicare and Medicaid Services (CMS) and the Joint Commission on Accreditation of Healthcare Organizations, healthcare providers must have the necessary practice credential. If healthcare organizations fail to follow the CMS regulations, they are not considered eligible for Medicare or Medicaid reimbursement.
Why is medical credentialing important?
The credential process for healthcare is essential because it enables patients to build trust in their physicians. Patients can be assured of the credentials of their doctors due to health care credentialing software. Medical credentialing solutions use a standardized process that involves collecting health informatics like electronic health records, verification of the primary source, and committee review by health plans, hospitals, and other healthcare agencies. Additionally, a credentialing software solution conserves resources and minimizes errors through healthcare automation.
Medical institutions need to focus on long-term health goals for population health management across various locations. This means that they will need hospital medical staff credentialing that is quick and efficient. Healthcare providers will be required to move less-urgent cases out of hospitals to other settings as and when needed. Physicians will need to use a medical staff credentialing process that can be managed from any location for this to work. Medical staff and credentialing would ensure that doctors are licensed and deliver reliable care services, including telehealth and mHealth. A healthcare provider credentialing software assures patients of their healthcare professional’s accreditation and experience. It also helps to deliver efficient collaborative care and perform health analytics. Medical credentialing solutions are required to improve the efficiency of care, integrate care, and increase patient engagement.
How to select the right medical credentialing software?
Before you choose a credentialing management system, ask yourself these questions:
- Why are you thinking of using a healthcare provider credentialing?
- Do you have the resources needed to integrate software credentialing healthcare providers?
- What benefits are you expecting from medical staff credentialing software?
- Do you need the software credentialing medical providers software for one location or more?
- By when would you like to implement the medical staff credentialing software?
- Were you able to find good stakeholders and vendors who can help you set up the medical credentialing software?
- Who will be managing the functioning of the medical staff credentialing software?
5 must-have features of credential management software
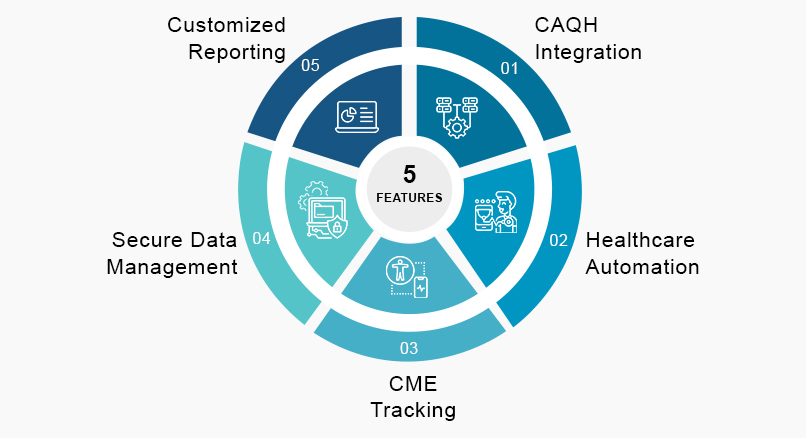
1. CAQH integration
CAQH (The Council for Affordable Quality Healthcare) is an online directory of credentialing data. Healthcare practitioners can self-report demographics, education and training, work history, etc., insurance companies can access that. The CAQH contains provider records and simplifies sharing of accurate information of physicians. Access to these electronic records with medical staff credentialing software can reduce the load of paperwork by eliminating the paper-based enrolment process involved with payer network enrolment.
2. Healthcare automation
Healthcare compliance credentialing gathers data from providers to create credentialing strategies, manage profiles, verify credentials, and contact payers. All these processes are performed through healthcare automation with cloud-based healthcare credentialing. Automation in the medical credentialing process can fasten workflow processes, including credentialing metrics and expiration management of credentials. Medical credentialing services can improve the efficiency of credential verification. However, some processes like acquiring diplomas or validating continuing medical education credits may need human intervention. Medical credentialing services reduce onboarding time and involvement for physicians, which improves satisfaction and experience with medical staff credentialing software.
3. CME tracking
Physicians are required to earn continuing medical education (CME) or Maintenance of Certification (MOC) points from time to time to continue practicing in their state and maintain their board certification. It can be cumbersome to keep track of CME credits and MOC points due to the hectic schedule of healthcare providers. Medical staff credentialing software can provide online CME tracking for monitoring credits in one place and helping physicians report to medical boards as and when needed. Credentialing software companies can help track the CME of healthcare professionals. Since learning among physicians may be a never-ending process, CME tracking is an important feature of medical staff credentialing software. It would be best if you chose credentialing software programs that simplify tracking and viewing CME certifications, credits, and scores. Medical credentialing for hospitals can automatically track CME, reducing the work pressure of performing these tasks manually.
4. Secure data management
Data containing credentials, certifications, training, and work experience can be huge datasets in practice management. It is important to manage data with such vital information through a safe platform. Manually handling and managing credentialing data can be time-consuming and challenging, not to mention the scope of errors with this approach. With a medical staff credentialing process, you no longer have to worry about these. You can store, segregate and view data securely with HIPAA-compliant medical staff credentialing software. Medical provider credentialing allows physicians and administrators to access credentials and other electronic records from anywhere, and rest assured that the platform would be secured.
5. Customized reporting
Creating custom reports is an important feature of credentialing in medical billing. Medical staff credentialing automates report making, which saves doctors time. Credentialing process in medical billing can help to reduce errors and fasten payment processing. Medical credentialing companies involve an ad-hoc writer to obtain necessary data and customize reports offering insights into the services delivered, days of enrolment, summary of institutions associated, etc.
Conclusion
Medical staff credentialing ensures patient safety, accurate analysis of medical records, reduces costs, and safeguards healthcare institutions from financial losses. Medical credentialing for hospitals validates the education, certifications, training, experience, and history of physicians. It is essential for keeping track of the credentials required by doctors to continue their practice. Medical staff credentialing software automates the entire credentialing process, which simplifies and fastens the cycle.
OSP can help you navigate medical credentialing and save you the hassle of managing all the documentation. We can ensure that the credentialing system is HIPAA-compliant, interoperable, and offers a secure platform for handling your important documents. Our cloud-based medical credentialing solutions can automate the application, primary source verification, credentialing, payer enrolment, and so on.
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.