Introduction
History has shown us that inefficiencies, deviations and a breakdown of workflow processes can pose a serious danger. The war veteran, who jumped the White House fence and made it past what was assumed to be the tightest security system for the first family, is one example. Not very long ago, the first person diagnosed with Ebola in the United States, Thomas Eric Duncan, surprisingly eluded detection at a Texas Hospital. We have seen many such lapses during the current COVID-19 pandemic as well. Blame game and finger-pointing aside, the bottom line is a failure of system workflow.
Healthcare organizations are consistently looking to overcome the challenges associated with quality of care, cost reductions, increased revenues. Optimizing processes and operational efficiencies are swiftly turning into a priority that can translate into increased ROI. Asset utilization is another challenge that needs to be addressed as patient numbers rise and physical capacity remains limited. Due to staffing shortages, the healthcare sector is battling overcrowding and a low level of satisfaction among patients.
Accessibility to data, low levels of automation, manual processes, complexities in billing and claims, reduced accessibility to relevant data are all workflow process challenges that translate to lower levels of patient satisfaction. Incomplete data in electronic systems, inaccessible paper formats, low levels of technology adoption, and paper-based systems further contribute to the challenges faced by healthcare organizations.
Automation of patient flow can go a long way in benefitting the healthcare provider and patients alike. Ranging from improved operational efficiency, higher patient safety, and increased quality of care, the benefits are immense. Ideally, an automated and efficient workflow management strategy would provide a patient with the best possible care, in the least amount of time and with the least amount of cost, which will translate into higher profits for the health provider.
Critical Factors Towards Establishing a Workflow:
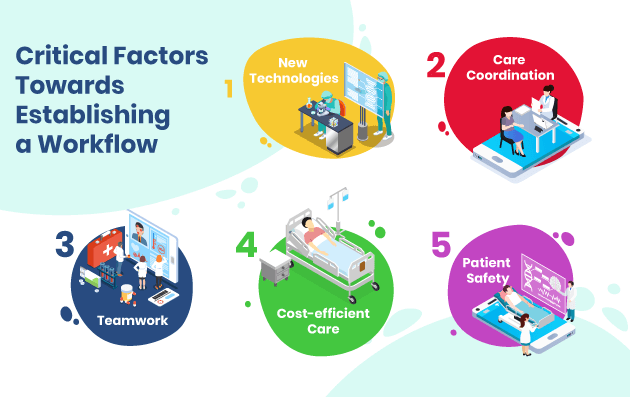
The key factors that a healthcare provider organization should consider when establishing a workflow include:
- New Technologies – Adoption of intelligent technologies can aid in streamlining workflow processes to provide higher quality care, improve organizational efficiency and satisfaction and create consistent processes that limit the possibility of operational errors. EHR systems allow for quicker response time and increased accessibility. Similarly, looking into automating multiple departments, with their relevant requirements, will aid in increased workflow efficiencies.
- Care Coordination – This includes follow-ups and related care for the chronically ill patients that, when automated, can reduce manual processes and increase patient satisfaction significantly. Furthermore, information lapses can be avoided, reworks can be minimized, and care-giving processes turn more consistent and reliable with compliance at its peak. The standardization of practice protocols translate directly into increased levels of patient satisfaction.
- Teamwork – Creating workflow processes that contribute toward the satisfaction and advantages of efficient teamwork is a crucial component of increasing overall quality of care. The processes should be implemented holistically across the organization, wherein processes are clearly communicated for the team to comprehend and achieve goals. Teamwork allow multi-department contribution for overall smooth functioning that can result in automated process handling.
- Cost-efficient Care – Workflow processes that work towards overall reduction of costs for the patient and organization, along with an increased ability to improve patient flow can contribute towards higher patient satisfaction and increased ROI. When manual paper-based systems are automated, the savings of the healthcare organization is drastically increased. Electronic processes reduce overall working costs and medical errors.
- Patient Safety – This is a crucial component of workflow efficiency that should remain high on the priority list, while establishing workflow processes. Measures to ensure patient safety, from contagious infections, etc. need to be factored in. Staff proficiency tracking is a strong enabler toward ensuring skill competency and process adherence. Clinical decisions are patient-centric that contribute toward successful patient engagement.
Common Mistakes to Avoid During Establishment of Workflow Patterns
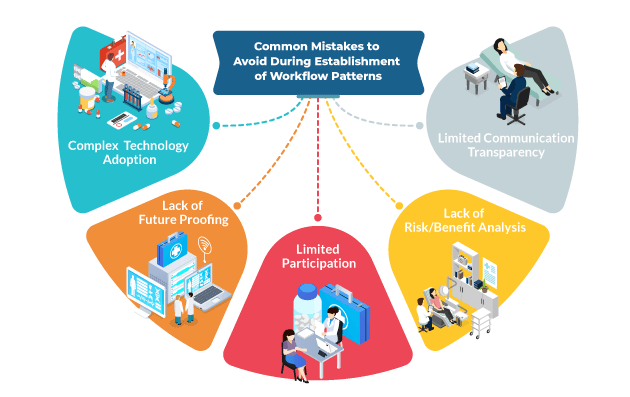
- Complex Technology Adoption – Enforcing complex technology adoption among employees can create a lopsided outcome. Technology solutions that are limited in their approach will pose more problems than solutions. From unauthorized usage, risk toward sensitive data, malfunctions, the complications will increase the burden on the organization and reduce productivity.
- Lack of Future Proofing – This is a commonly witnessed error across organizations that fail to factor in the changing landscape of the healthcare sector, along with the evolving requirements of their own organization. It results in limited technology implementation that cannot address the needs of added participants, systems and overall growth. Workflow system processes should be enabled with provisions for future developments.
- Limited Participation – When establishing workflows, it is important to look at enablement as holistically as possible. If participation is limited to certain individuals, it reduces the efficiency of overall functioning and places the burden on some as opposed to overall teamwork. Higher usability creates a larger adoption level and increased productivity. Security controls can be put in place, but accessibility should be looked at generously.
- Lack of Risk/Benefit Analysis – Workflow processes should not be driven purely by IT, but rather from the clinicians and patient’s perspective. An IT-centric approach will create a gap between the organizations’ on-ground needs and the reality of adoption. A clear risk vs benefit analysis and usability testing process should be undertaken before implementation to ensure comprehensive integration across the organization.
- Limited Communication Transparency – Adopting an inclusive approach during decision-making and planning of workflow processes is the key to successful implementation. When decisions are made in isolation from the operational staff, adoption can suffer through employee hesitation. Free and open communication will allow for both perspectives, between stakeholders and staff, to be incorporated.
8 Essential Elements to Elevate Clinical Workflow
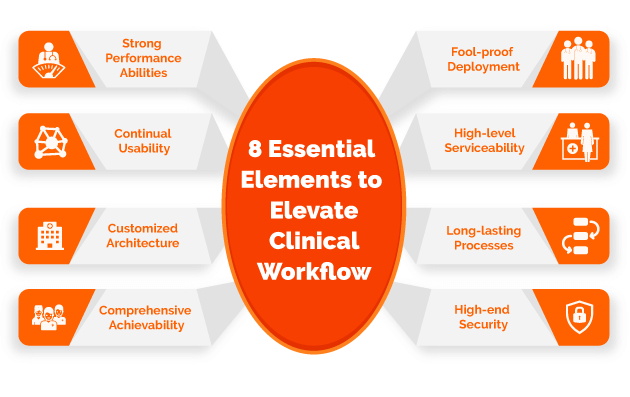
An optimal workflow model involves carefully thought out strategies. Listed below are the key strategies that should be prioritized.
- Fool-proof Deployment – The workflow strategy that is finalized should be crossed checked for errors and loopholes before implementation. There must be complete reliability on the infrastructure.
- High-level Serviceability – This is an assurance that the infrastructure involved in the workflow will adhere to comprehensive serviceability between staff, physicians, patients and third parties.
- Long-lasting Processes – Whatever the extend of your deployment toward workflow efficiency, the investment will be worth it if the processes are durable and can be consistently operated for an extended period of time.
- High-end Security – Specific to the healthcare sector, security is a foremost concern and should be at the top end of our perspective toward any technological adoption. Strict security measures, that protect patient data, are mandatory.
- Strong Performance Abilities – Given the high level of pressure and demand on healthcare organizations, the ability of performance needs to be at par. A successful workflow model should function across multiple devices and platforms.
- Continual Usability – The workflow infrastructure should be designed in a fashion that takes into account, not only the current requirements, but has provisions for future needs as well.
- Customized Architecture – Among the healthcare sector, organizations have varied needs and a ‘one size fits all’ model is bound to prove inefficient. The deployment should carefully consider the specific needs of the organization.
- Comprehensive Achievability- This refers to a model that is constructed with a holistic vision to achieve the whole spectrum of goals of the organization – from improving operations, to reducing costs, to providing higher staff and patient satisfaction.
Hospital Workflow Strategies for Better Patient Outcomes

- Focused Collaboration: This involves a strategy that takes into account multiple viewpoints from across the organization that will extend itself toward broad-spectrum adoption.
- Target Specific Bottlenecks – During the stage of planning for a workflow optimization model, keep your initial focus on complexities that currently exist and the processes thereof.
- Careful Technology Investment – Among the multiple options available, it is prudent for every organization to evaluate their specific needs and adopt technology that addresses those requirements.
- Opting for a Redesign – For overall efficiency, it is usually prudent to start from scratch and redesign the entire workflow architecture. This can address bottlenecks and also add processes for improved results.
Features of an Optimal Workflow:
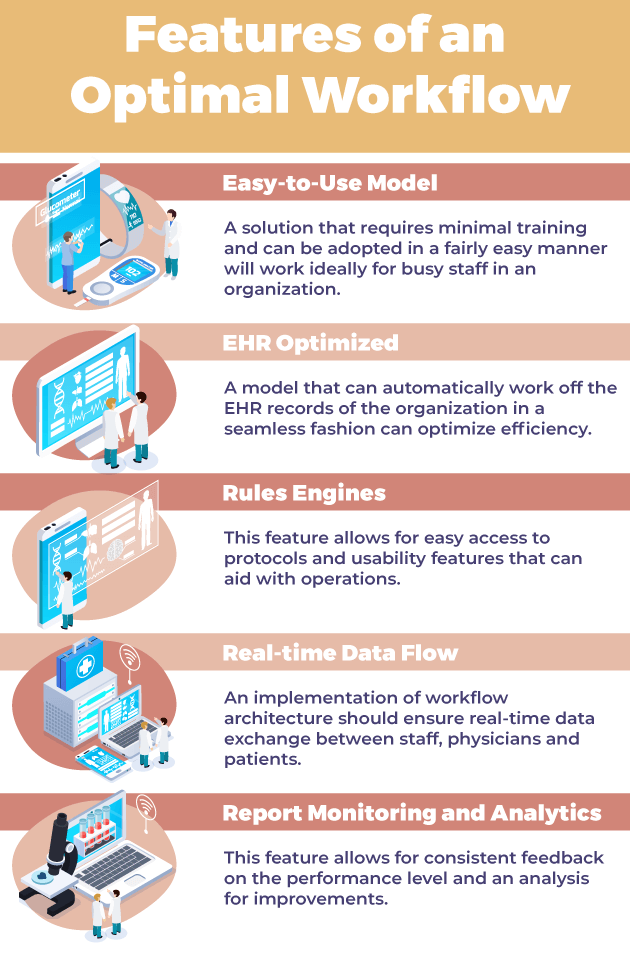
- Easy-to-Use Model – A solution that requires minimal training and can be adopted in a fairly easy manner will work ideally for busy staff in an organization.
- EHR Optimized – A model that can automatically work off the EHR records of the organization in a seamless fashion can optimize efficiency.
- Rules Engines – This feature allows for easy access to protocols and usability features that can aid with operations.
- Real-time Data Flow – An implementation of workflow architecture should ensure real-time data exchange between staff, physicians and patients.
- Report Monitoring and Analytics – This feature allows for consistent feedback on the performance level and an analysis for improvements.
Conclusion:
The adoption of a healthcare workflow strategy includes multiple factors such as staff empowerment, workload anticipation, productivity management, and overall automation tools. As healthcare organizations cope with unprecedented pressure, these strategies are critical toward success.
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.