The healthcare sector is a service-providing industry, where patients are the main focus. However, the revenue cycle forms an essential component of healthcare, where many providers struggle. Effective medical billing and reimbursement demand that healthcare leaders communicate well and work together to manage the revenue cycle. A poor reimbursement system can lead to loss of revenue, and this is the last thing any healthcare provider would want. When it comes to healthcare reimbursement, medical professionals are faced with a growing entanglement of government regulation and payer policies.
Digital and technological revolutions in healthcare have transformed healthcare reimbursement systems. Manual health insurance reimbursement is now automated, which reduces labor costs and avoid claim denials. Healthcare technology is much needed today to prevent errors in health equity reimbursement and promote better revenue generation.
How healthcare technology is improving care delivery
Health informatics offers opportunities for improving health care reimbursement. Value-based reimbursement technology consists of simple charting, advanced decision-making, and integration with medical technology. Reimbursement systems reduce human errors, improve clinical outcomes, facilitate collaborative care, enhance practice management, and analyze medical records management over time.
The reimbursement system in healthcare also serves as useful for telehealth and mHealth practices. Digital technology has enhanced operational efficiency while maintaining HIPAA compliance at the same time. The digital transformation has simplified reimbursement in medical billing and improved patient engagement. Technology in healthcare has made it easier for doctors to manage hospital reimbursement and receive payments for all the hours invested.
The topmost five healthcare technologies for improving reimbursement
Claims processing in reimbursement systems can speed up the medical billing process and the entire revenue cycle. These five technologies can help healthcare providers with healthcare insurance and reimbursement.
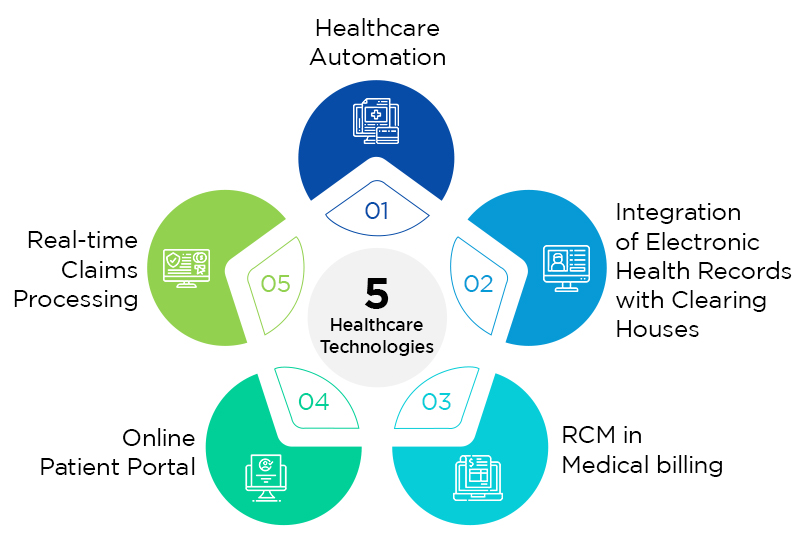
1. Healthcare automation
Automating a reimbursement system in healthcare track and capture revenues associated with delivering services to patients. The revenue cycle consists of many areas, such as patient pre-registration, eligibility verification, clinical visit, claim coding, medical billing, denials management, and payment collections. Each of these processes includes tasks usually manually conducted by administrative staff, which can slow down the entire cycle. Not only that, manual processes in medical billing are labor-intensive, expensive, and subject to errors.
As medical systems integrate technology, healthcare reimbursement systems’ automation needs to be more efficient with billing accuracy. Healthcare automation fastens the entire billing cycle and can be applied even for integrated care services. Automation in healthcare begins when patients leave a clinic or hospital. Reimbursement in healthcare from insurance companies is dependent on the efficiency of billing automation. Medical coding and billing automation can significantly improve Medicare home health reimbursement. From appointment scheduling, registration process, billing, and coding, automation in reimbursement mechanisms for healthcare govern the costs incurred.
2. Integration of electronic health records with clearing houses
The introduction of digital technology in the reimbursement system in healthcare is a blessing when managing electronic health records. Healthcare reimbursement models eliminate paper works and loss of patient medical records. Electronic health records make it easier for clearinghouses to electronic exchange data and process the healthcare reimbursement system. Patient records can be accessed from anywhere and result in better health outcomes. EHRs also simplify and fasten reimbursement solutions. EHR in clearinghouses can help reduce the number of open patient accounts within a short period. Health care reimbursement solutions avoid delays in claim processing and prevent claim denials. EHRs can decrease the time spent on paperwork and make it easier to transfer data across different systems. Administrative tasks such as form filling and processing billing requests represent a significant percentage of healthcare costs. EHRs can enhance practice management efficiency by streamlining the tasks and decreasing the costs.
EHRs integrated with clearinghouses can enable the smooth functioning of the billing and administrative departments. The billing department won’t have to stop working on one program and open another to find the specific data, and there is no need to enter data manually and repeatedly. It also increases the efficacy of a reimbursement system in healthcare to increase revenue. Due to EHRs, patient data are quickly accessible, making it easier for practice management software to obtain claims and submit them to the payers.
3. RCM in Medical billing
Healthcare practices need to integrate revenue cycle management for reimbursement systems in healthcare to make sure they receive the payment for the care delivered. Managing denials, increasing collections, and resubmitting claims are accomplished by RCM in medical billing. However, to make the most out of a healthcare reimbursement plan, the RCM strategy must track key billing metrics and follow best practices for revenue success. Medical billing key performance indicators (KPIs) help healthcare practices keep track of financial health with healthcare payment reimbursement solutions. It is essential to identify the KPIs with healthcare reimbursement and payment systems to understand the financial performance, recognize any problem areas, determine healthcare revenue fluctuations, and implement population health management.
4. Online patient portal
Medical billing reimbursement solutions can be enhanced with online patient portals that allow patients to access their accounts and make payments easily. Patients can pay bills online through patient portals, and physicians can track the payments. This decreases delays in a health care payment system. Online patient portals also improve patient-provider communication and increase patient satisfaction. When it comes to payment and billing, it saves time and improves the efficiency of value-based reimbursement models in healthcare. Value-based reimbursement through online patient portals is convenient and secure. If healthcare providers can encourage patients to use portals, they are likely to return for your services. Online patient portals support faster payments through a secure gateway. These portals can save both your time and money by automating administrative tasks.
5. Real-time claims processing
Real-time claims processing is one of the reimbursement challenges in healthcare. Technology has made it possible to process claims in real-time and speed up eligibility checking. It is essential to know if or not a patient’s insurance covers a particular process in the treatment. This knowledge is crucial for reimbursement systems in healthcare. Advanced value-based models in healthcare make it possible to perform real-time claims processing. Real-time claims processing with a reimbursement system in healthcare reforms how healthcare claims are submitted, remitted, and paid to improve the billing cycle’s efficacy. Healthcare staff no longer need to go through tons of paperwork and wait for long durations to process claims.
Changes in Healthcare Reimbursement Models
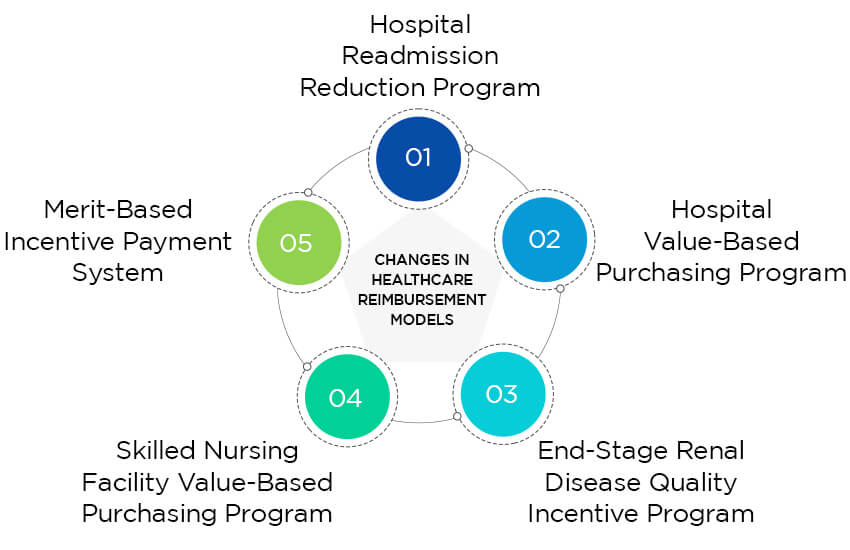
The most dramatic shift in the healthcare reimbursement model is the transition towards value-based care. Value-based care sees quality over quantity. And physicians and hospitals under this model are paid according to the quality of care rendered. Value-based care emphasizes preventive care more to keep hospitalizations and revisits to the minimum. It also helps providers reduce the emergence of hospital-acquired infections and readmissions post-surgery.
Interestingly, this healthcare reimbursement model rewards clinicians for providing quality services to a community or patient population. And those practices unable to meet the quality expectations are penalized.
Some of these Medicare value-based care programs include-
- Hospital Readmission Reduction Program: This program incentivizes hospitals if they reduce readmissions and HAIs.
- Hospital Value-Based Purchasing Program: This program measures and scores hospitals on improving patient experience, reducing hospital errors, and implementing evidence-based care.
- End-Stage Renal Disease Quality Incentive Program: This program is specifically for dialysis providers. It scores them and reduces their payment if quality requirements aren’t met.
- Skilled Nursing Facility Value-Based Purchasing Program: This program is specific to nursing and nurse-based facilities. It rewards facilities that meet the CMS quality requirements.
- Merit-Based Incentive Payment System: Under this program, CMS rewards physicians with a bonus for quality improvement and cost. And for poor performance, they’re penalized.
The focus of insurance companies has also begun to change toward value-based healthcare reimbursement models. Value-based care played a crucial role in motivating hospitals and other providers to explore new healthcare access and quality solutions. These ideas are intended to lower healthcare expenses while enhancing patient health.
Key Trends in Healthcare Payment Systems 2023
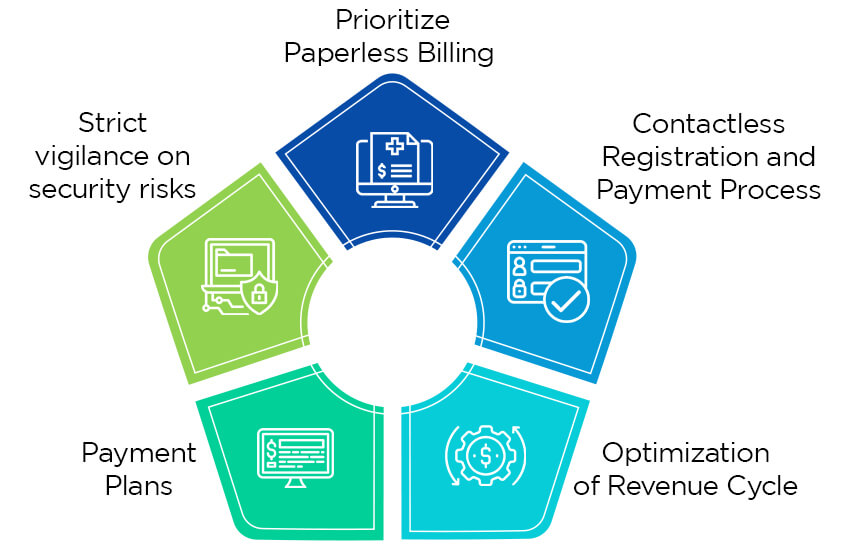
1. Prioritize Paperless Billing
Paper bills will soon be outdated. As per a recent healthcare payment survey, nearly 70% of consumers receive their medical bills via mail, but only 9% prefer to pay them by paper check. Almost 91% of them wanted electronic payment methods. Delivering patient bills electronically saves time and money compared to sending numerous bills before receiving payment.
Many industries employ and accept paperless billing, often known as electronic statements or eStatements. Although many medical practices provide eStatements as a billing option, adoption still needs to be improved. Making eStatements, the preferred or default billing option can encourage its adoption. Encouraging patients to sign up for eStatements by sending them via email or text message, even before appointments, will enable you to avoid mailing them a bill.
2. Contactless Registration and Payment Process
Today’s consumers want to feel self-sufficient. And digital tools are the only way to make them feel that, and this includes healthcare reimbursements as well. However, there is a huge gap between provider and consumer attitudes toward digital options. A recent report highlighted this quite well. According to this report, nearly 40% of providers think billing and collection have zero impact on patient experience. On the contrary, 49% of consumers said they would prefer a provider who can provide a seamless payment experience.
With digital health tools, this scenario can improve drastically. Encouraging providers to ensure registration and payment process via online channels can boost patient experience and attract more consumers. Providers must choose an IT vendor with a track record of introducing cutting-edge payment technology and be aware of the inherent complexity of the payments and healthcare industries.
3. Optimization of Revenue Cycle
Optimizing the revenue cycle from time to time can ensure that funds are available when required. The current trending way to optimize the revenue cycle is to adopt electronic registration and payment methods and offer diverse payment plans. These can generate revenue as per the point of service and even minimize the AR cycle.
Another crucial factor is how quickly healthcare groups can access their funds. Funds received by an organization the same day or the following business day can be managed more effectively and provide real-time visibility into cash positions. Healthcare managers should assess their company’s revenue cycle to find strategies to increase cash flow and boost employee productivity.
4. Payment Plans
Medical costs can be overwhelming, and they will continue to be. According to a report, nearly 75% of people with health insurance worry about the financial hardship of their medical bills, and many others delay the care until they’ve money. Offering payment plans may remove this concern and allow people to pay over time. Payment plans provide visibility into future cash flows and some level of assurance regarding whose amounts will be paid. And this could be why more practices are presenting this choice.
5. Strict vigilance on security risks
The Office of Civil Rights report reported over 700 healthcare breaches of more than 500 records. And that resulted in maligning the privacy and security of over 50 million patient records. With many potential entry points across software systems and valuable personal information that can be used to construct new identities, the healthcare industry remains a desirable target for cybercriminals.
Millions of dollars in real and brand costs are lost due to a cyberattack. Medical practices must search for third-party service providers with certifications from compliance and payments security groups and healthcare standards organizations.
Conclusion
Healthcare technology has transitioned many processes, including medical billing and payment processing. Cloud-based healthcare reimbursement forms a major component of care service delivery, and interoperable technological systems simplify this. The reimbursement system in healthcare manages claims quickly and without errors. OSP can help you choose the right healthcare technologies and create custom solutions as per your requirement.
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.