Introduction:
Medical billing mistakes can be easily made but have drastic repercussions on the overall profit of the healthcare organization. Returned claims with errors, denied claims, rejected bills, incorrect coding, and insufficient data are just a few of the many woes of poor revenue cycle management in healthcare. Almost 30% of medical bills are prone to medical billing errors. As common as these issues are, as complex as the system may be, the solution is at hand. As we sort through the commonality of medical coding errors and how to prevent them, how to correct medical billing errors, and steps in the medical billing process, certain areas reveal a gaping hole. Improper medical billing can be mitigated through healthcare revenue cycle management solutions.
As medical billing and coding errors increase in frequency, patient experience is diminished, profits are adversely affected, and the overall revenue cycle for healthcare is shunted. Efficient provider revenue cycle management can evade these outcomes through accurate claims management, offered through practice management solutions.
How We Built a Successful RCM System?
At OSP, A Texas-based mental health center wanted to automate the manual medical billing process. Paper-based practice management and the RCM cycle in medical billing were causing a loss of revenue and diminishing the quality of care. The main challenge for OSP was to bring in the digitization of the clinic’s daily practice and revenue operations.
We built a comprehensive revenue cycle management healthcare solution to offer:
- Digitized Credentialing
- Document Expiration Alerts
- CAQH Management
- Co-pay Management
- Online Payment
- A/R Management
- HIPAA Compliant Solutions
- Secure Patient Data Management
- Secure Cloud-based System
- Telehealth Appointment Management
- Patient Engagement System
The Process – Steps of Healthcare Provider Revenue Cycle Management
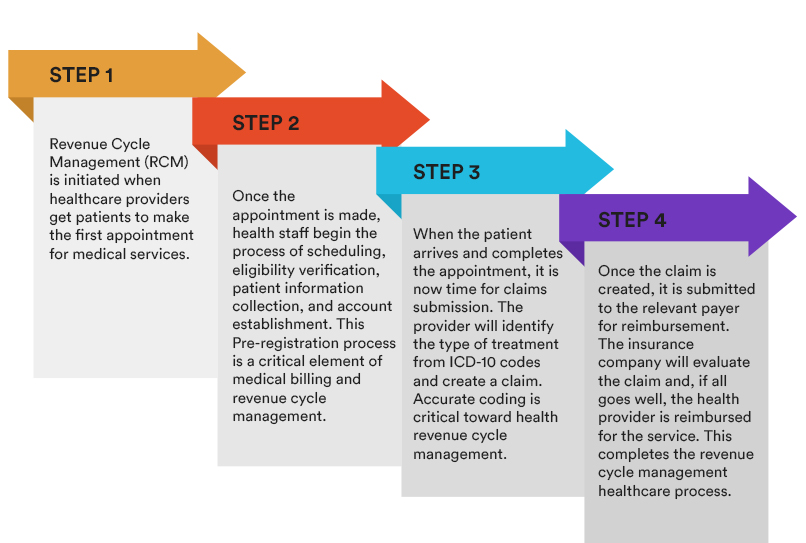
Step 1: Revenue Cycle Management (RCM) is initiated when healthcare providers get patients to make the first appointment for medical services.
Step 2: Once the appointment is made, health staff begin the process of scheduling, eligibility verification, patient information collection, and account establishment. This Pre-registration process is a critical element of medical billing and revenue cycle management.
Step 3: When the patient arrives and completes the appointment, it is now time for claims submission. The provider will identify the type of treatment from ICD-10 codes and create a claim. Accurate coding is critical toward health revenue cycle management.
Step 4: Once the claim is created, it is submitted to the relevant payer for reimbursement. The insurance company will evaluate the claim and, if all goes well, the health provider is reimbursed for the service. This completes the revenue cycle management healthcare process.
The Challenges – Traditionalism in Provider Revenue Cycle Management
- Healthcare compliance and regulations are continually changing and evolving. It is, therefore, difficult for health facilities to maintain a stable physician revenue cycle management policy.
- Due to system hurdles, collecting the payments from patients before or at the point of service has become increasingly difficult.
- Non-payment of medical bills by the patient increases the number of deductibles and creates a financial strain on the healthcare organization.
- Striking a balance between ensuring that debts are collected while also preventing patients from seeking out competitive medical providers is complex.
- Manual eligibility processes are prone to errors, and patients often do not understand their coverage options.
- Tracking a claim through its entire lifecycle is a time-consuming process and requires additional staff for solely this purpose.
- If not caught immediately, errors in billing can cause significant back and forth and delay the entire payment process.
- Unidentified errors result in denied claims, which lead to a lack of revenue and decrease the bottom line of the health facility.
- Training health staff toward physician revenue cycle management has turned into a pain point for healthcare organizations due to the job’s complexity.
The Future – Essential Features of Healthcare Revenue Cycle Management Solutions

1. Cloud Presence:
The future of healthcare provider software solutions is cloud-based solutions. A revenue cycle management solution is no exception. A solution on the cloud means that the health facility’s IT department no longer has to worry about space and bandwidth issues toward accessibility. Cloud computing in healthcare provides 24/7 accessibility of the solution without restrictions of space and hours. Medical records management is simplified when there is no stress about limits on data and accessibility. Another significant advantage of cloud-based RCM software is accessing electronic health records, even if the local system fails. This maintains patient data security from being lost through secure back-ups. Finally, if the system needs to be accessed across multiple locations, cloud-based access to integrated healthcare solutions is the best option.
2. Comprehensive Training:
RCM healthcare provider solutions should offer holistic denial management RCM training for the system for multiple functions. Training of healthcare staff in the organization should be organized in batches, and the revenue cycle management vendors should be prepared to offer the same. Organize the training in a manner that places the tech-savvy and relevant staff at the top of the list to address gaps in understanding at a later stage. Revenue cycle management services for healthcare should offer a demo of the customized software to ensure that all the services required will be present in the final version. This will eliminate development delays along the way. Additionally, incorporating healthcare analytics solutions within the RCM software will ensure advanced capabilities for the healthcare organization.
3. Highest Value Submission:
The goal of every healthcare organization is to maintain high profitability through healthcare automation. An essential factor in achieving this goal is ensuring that claims are submitted at their maximum value through medical informatics. Revenue cycle management for healthcare providers can be successful based on the criteria of highest value submission. When this policy is embedded into the RCM software, it can neutralize the effect of potential reductions in reimbursements since the value of the claim is at its highest potential. A well-integrated hospital-based physician RCM solution can better track claims values and not allow errors to slip through the cracks. Manual intervention is minimal, claims are processed faster through electronic data exchange, and the healthcare facility can expect a better bottom line.
4. Eligibility Verification:
The manual task of patient eligibility verification is cumbersome. Patients are routinely moving across different insurance coverage providers or to other plans. An automated and advanced RCM solution will swiftly manage the eligibility of patients with minimum manual intervention required. Data transactions can be conducted online to limit the complex processes of phone calls with patients and insurance agencies. Provider solutions for revenue cycle management hold automated checks of authorizations; patient responsibility amounts to optimally analyzing co-payments.
5. Tracking and Modification:
During the coding process, there is always a possibility of errors. Coding error possibilities are much higher when the process is undertaken manually. Incorrect coding rectification takes a long time and can affect overall healthcare management. Therefore, one of the most preferred providers revenue cycle management solutions features is automated coding and tracking. The process of automated coding restricts the possibility of errors. Even if there is a case of incorrect coding, real-time tracking and monitoring of status will highlight the error right away. Prompt modifications can then be undertaken for immediate rectifications.
6. Denial Alerts:
Another essential feature of futuristic RCM solutions is denial alerts. The easiest way to mitigate denials is to opt for an automated feature of predicting denial possibilities on the RCM platform. Through this capability, denied claims are flagged for immediate resolution, and any member of the medical billing team can quickly resolve the matter through re-coding. Through this ability of provider revenue cycle management solutions and healthcare interoperability, worker productivity increases, and a seamless payment processing flow is maintained across the organization.
7. KPIs and Reports:
An analysis of the revenue cycle management system is an analysis of the overall health of the organization. Therefore, periodic reports and Key Performance Indicators (KPIs) can be considerably beneficial when they are readily available for staff meetings and other purposes. A revenue cycle management provider software that can offer these reports in an automated and periodic fashion can boost the financial health of the practice to a large extent. Other factors, such as population health management, can also be included in these reports for additional gain. Weekly reports and KPIs can consist of relevant documentation, an analysis of timely completion of billing-related jobs, insurance protocols, and financial reports.
How Does Revenue Cycle Management Benefits Providers?
Healthcare providers prioritize quality patient experience and care the most. But that doesn’t only mean providers have to treat patients rightly; it’s also about effectively managing administrative tasks that lead to timely reimbursements. And for that, providers resort to healthcare revenue cycle management systems. Implementing this revenue cycle management software offers a myriad of benefits. Take a look at these most common benefits of using healthcare revenue cycle management for hospitals or independent practices.
1. Maximum Claims Cleared after First Submission
Ensuring clearance of claims after the first submission is crucial as it can save providers from costly delays. Nearly 5 to 10% of claims are denied after the first submission. And the most common reasons are coding errors, insurance verification issues, and missing patient information. These are all technical and human errors that can be easily prevented.
With provider revenue cycle software, the focus on front-end tasks is more, meaning claims are paid only after the first submission. Front-end tasks include insurance verifications, patient information collection with high-end accuracy, and proper coding. Providers no longer need to wait for claims clearance after the first submission, as 90% of claims denials are now preventable.
2. Improved Collections and Revenue
Healthcare practices undergo severe losses due to delays and denials of claims. Of course, they need to pay for services they offer to patients and even staff for their work. But when claims don’t get clearance and money is not reimbursed, healthcare practices find it extremely difficult to manage their expenses.
However, hospital revenue cycle management can effectively resolve this issue by identifying the pattern of denials. Identifying the denial patterns can help providers to take effective measures to overcome the issue and get paid on time. Such healthcare revenue cycle solutions can help providers generate an additional $5M on average.
3. Reduced Administrative Burden
Healthcare providers are already exhausted from delivering their care services. Additional administrative tasks are just overwhelming for them. When a patient book an appointment, providers are responsible for scheduling the appointment with the physician, collecting and entering patient information, and verifying insurance. All these tasks consume a lot of time and shift their focus from patient care. However, the revenue cycle software for providers can change this but automating these processes.
Healthcare revenue cycle solutions take care of these initial tasks to ensure accuracy and faster clearance of claims. Automating these processes will help providers to focus mainly on patient care while they get payments without any hassle.
4. Increased Attention to Quality Care
When providers don’t need to stress over claims delays or denials, they can spend more time improving the quality of care. This is possible by implementing healthcare revenue management solutions to ensure accuracy and effective claims submission. And providers need to not spend a penny on correcting errors and resubmissions. They can spend more on improving the quality of care. Moreover, RCM solutions can also help providers to switch to value-based reimbursement models and optimize their financial status.
5. Prevent Patient and Healthcare Fraud
Patient frauds often happen due to incorrect information given by patients or medical identity theft. In both cases, providers are at a loss as such situations cost providers a lot of money. Besides, healthcare fraud also impacts providers’ revenue a lot. Incorrect coding in billing can lead to healthcare fraud, which may be intentional or unintentional. It can be due to billing of services not rendered, charging for unnecessary procedures, care service given by unqualified employees, and low-quality care.
However, revenue cycle management in healthcare saves providers from both types of fraud. RCM solutions identify errors, verify patient information and ensure accuracy in coding to help providers save money and lower their fraud risks.
6. Enhanced Patient Experience
From the chores that the RCM application does, it’s clear that providers can focus more on patient care that directly impacts the patient experience. As RCM automates the process of scheduling and filling out intake forms, patients and administrative staff are satisfied and feel relieved. Moreover, the software solution also takes care of insurance eligibility checks, which means patients need not face the hassle of payment issues later. With all these tasks taken care of by the revenue cycle management process, an enhanced patient experience is guaranteed.
Optimize Provider Revenue Cycle Management- Best Practices
Revenue cycle management in hospitals follows a simple track- it starts when patients book an appointment and ends when the hospital receives the payment. However, revenue cycle management can be optimized by adopting some of these best practices.
1. Avoid Physician’s Enrolment Issues: One of the crucial issues that lead to revenue problems is physician credentialing and enrolment. Practices tend to neglect this, considering this unimportant. But in reality, failing to ensure credentialing and enrolment can cause delays in payments, increased denials, healthcare fraud, and whatnot. It’s always better to dedicate time and resources to ensure these tasks to avoid any revenue mishaps later.
2. Manage Denials: Mitigating claim denials must be a priority for providers. And revenue cycle software solutions are great at doing this. Claims are often denied due to a myriad of reasons. Be it coding errors, duplicate claims, eligibility and filing issues, missing or incorrect information, etc. It’s essential to track the claims process to understand the reason for its denials. RCM solutions usually take care of this by closely monitoring the claims process and understanding the pattern of denials. And help providers to prevent denials further.
3. Manage ARs: Increased ARs under 90 days indicates good cash inflow. Providers are often suggested to keep track of the percentage of ARs over 90 days, indicating the facility’s ability to collect payment timely. Several factors determine a stable revenue cycle and timely payments, including staff’s efficacy in managing denials and old claims, payer mix, and patient payment collection capabilities. RCM software is quite effective in ensuring that the percentage of AR is over 90 days. Moreover, it helps analyze the denied claims and compliance time-to-time to avoid losses.
4. Track Days Revenue Outstanding: Days revenue outstanding means the number of days a provider/healthcare facility takes to collect due payments on average. Using revenue cycle services to track the day’s outstanding revenue is a great practice. Moreover, the fewer days, the faster the payment collection. Typically, a practice must keep it within 50 days to ensure a healthy revenue cycle.
5. Track Financial Performance: Healthcare practices are doing well with a consistent cash flow rate. It indicates the financial stability of the practice. Moreover, monitoring the different KPIs regularly can help understand and improve the practices’ financial performance. And KPIs that practice can consider monitoring are net collection rate, AR analysis, Days Revenue Outstanding, and charge posting and billing lag analysis.
Conclusion
Provider revenue cycle management solutions have evolved to a large extent to accommodate the dynamics of healthcare organizational financial needs. Provider solutions in revenue cycle management can now streamline the entire lifecycle of financial and medical processes and provide accuracy like never before. Technological advancements are deployed to track claims, collect payments, and resolve denials. Consequently, these solutions contribute significantly to generating a continual flow of revenue. As hospitals and other healthcare facilities actively incorporate provider solutions for revenue cycle management, it would be prudent for every health facility to analyze its particular demands. A customized solution is generally the best fit.
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.