Contents
1. Introduction
A person’s medical history speaks volumes about their health, and it tells consulting physicians what to look for and how to treat the patient. This is especially true for people who suffer from chronic conditions like diabetes, heart disease, or serious illnesses like cancer or an autoimmune disease.
Loss of a patient’s medical records, either partially or completely, could have a major impact on his or her treatment, and not in a good way. It’s the main reason for stringent laws to protect people’s medical information privacy and integrity. A single fact about a person’s family history could shed new light and help doctors treat him/her with greater effectiveness.

It became important for doctors and medical staff to view them as quickly as possible when a patient comes in. It’s especially vital if it’s a medical emergency. So, when patient details were digitized for the first time, it was a boon for doctors and patients. Physicians could quickly access their patients’ complete medical information and make informed decisions about urgent treatments. So, electronic health records were an important piece of tech adoption that impacted the healthcare industry.
Electronic health records (EHR) help both doctors and medical staff perform their work faster and more efficiently. So, let’s discuss how the integration of EHR helps hospital workflows.
2.What is EHR?
We’ve all heard of EHR when talking about healthcare. This section will go into the details of what it exactly is and how it helps both patients and providers alike.

EHR (electronic health record) is ubiquitous in healthcare in the United States. Simply put, it is an electronic form of peoples’ medical history that the provider maintains. It would contain all of the clinical information about people when under care by a certain provider. Some of that data would include immunizations, allergies, test results, radiology reports, history of treatments and medication, diseases and injuries sustained, prevailing medical conditions, and so on. Electronic health records make it vastly easier for doctors to access important medical information and help to simplify clinical workflows.
The chronology of a patient’s health situation, underlying conditions, previous diseases, or medication enables doctors to make informed decisions about treatment. EHRs make it convenient for doctors to obtain patient information quickly, share it with other organizations, and update the treatment.

A major advantage of having medical records in digital format is that they can be incorporated into other healthcare management solutions that help streamline hospital workflows. Medical staff at a clinic could access it with a few clicks and carry out medical coding and submit medical claims faster. A physician seeing a patient remotely through a telehealth application could pull up that patient’s electronic health records in seconds to help with the consultation.
EHRs make it easy to store, access, update, and manage the health information of millions of people countrywide. This also offers the benefit of aggregating large amounts of clinical data to enable superior population health management and improve upon existing treatments. In other words, electronic health records have made it a win-win for all stakeholders involved – the patients, healthcare providers, and healthcare payers.
3. Difference Between EMR and EHR
Many people use the terms Electronic Medical Records (EMR) and Electronic Health Records (EHR) interchangeably. But for professionals in healthcare and associated policy-making, the two are not to be confused. While the difference might just be in one word, the actual difference between the two is considerable. In this section, we’ll explore how the two terms differ.
If you’ve been involved in healthcare in any capacity in the United States, you had to have heard the acronyms EMR and EHR used extensively. For most people, the two mean the same thing. But it is not so for healthcare professionals.
EMR stands for electronic medical records. In this context, the word “medical” means the things concerned with medical procedures, usually those involving treatments and diagnostics. On the other hand, EHR stands for electronic health records. Here, “health” is a broader term covering a lot more. In simple words, health refers to a state of being sound in body and mind and being free of diseases. In light of this, it is agreed upon that EHRs are more comprehensive than EMRs.

EMRs are a digital version of the physical reports contained in a physician’s clinic or a single healthcare organization, including a patient’s medical history and previous treatments. An EMR enables a doctor to view a few factors regarding a person’s overall health, such as blood sugar levels, immunizations, etc. But it’s not easy to send an EMR from one practice to another.
An EHR can do a whole lot more than EMRs. They offer a complete 360-degree insight into a person’s health state. Moreover, they are also made to be shared amongst the broader medical community. In other words, if the EHR of a certain patient is collected at a hospital, it can also be shared with specialists at other hospitals, ambulatory care centres, testing centres, and so forth. Subsequently, all the experts can update the EHR as per their findings, recommendations, treatment, and prescriptions. The biggest advantage of an electronic health record is that it can be created, viewed, managed, and updated by multiple specialists across different organizations involved in a patients’ care.

The patients themselves can also access eHRs, and they follow the patient to different organizations, states, and even countries. The benefit of such flexibility is that it empowers caregivers to collaborate on unusual cases and requires an atypical approach and a collective effort by a team of multi-specialists. This is especially helpful for people who suffer from rare disorders and for whom conventional treatments only produce limited results.
As a person’s care journey progresses, the information and results are updated to reflect changes in his/her health. All the clinicians involved in the care of that patient can access the updated information in the EHR and stay abreast of any developments. Moreover, the patient can access his/her health data too and participate better in the care. With these benefits, an EHR is immensely helpful during follow-up care, such as post-surgical therapy or consultations. Additionally, electronic health records also make it easy for doctors to move patients from one care setting to another without endangering their health or disrupting a course of treatment. It’s only a matter of transferring patient records to the other organization’s digital system to enable doctors to access it.
So, EHRs are more than just a digital copy of a person’s medical charts.
Conclusion: they are crucial for doctors to better understand the overall health condition of a patient and make informed decisions. This factor goes a long way in improving patients’ medical outcomes involved in serious, life-threatening accidents. When such patients are brought into the emergency room, they’re likely to be unconscious or unable to provide any details about their health on their own. When the attending doctor can access such a person’s medical history, he would know everything about the patient’s allergies, history of medication, presence of diabetes, high blood pressure, heart disease, pregnancy, and so forth. This information is crucial in making informed decisions that will save the person’s life or reduce risks for the surgeons by eliminating uncertainty.
In addition to helping clinicians get a complete view of patients’ health, electronic health records also help experts in public health assess medical information from a large number of patients. This is indispensable when fighting a pandemic, as experts can help understand the disease and its symptoms, enabling policymakers to implement measures to contain the spread of infection. In other words, EHRs are an amazing tool for improving the overall process of population health management.
4.What Do EHRs Contain?
We’ve talked about EHRs and how they have had a positive impact on the overall care delivery process. But what is the information they contain that allows doctors to work better? This section talks about the data in EHRs that helps with the treatment.

The health information in EHRs assists doctors in administering the correct medication and improving the overall patient outcomes. In chronic conditions such as heart disease and high blood pressure, EHRs make it easier for doctors to help patients manage their condition better. Let’s have a look at what an EHR contains –
1. Medical Data
A person’s medical information tells doctors about the history of his or her medication. The pills consumed give an idea of the person’s health situation since they’re specific. For example, medicine for thinning blood indicates that a person suffers from high blood pressure; a person taking insulin says that he/she suffers from diabetes.
This data is coupled with the timelines since it is necessary to know when to take which medication. Things like the history of smoking, alcohol, or substance abuse are extremely important to be included. Prescriptions from previous doctors on record also help. The more thorough this data is, the better it is for treating physicians to know the right dosage for current conditions.
2. Identification & demographic info
This is one of the first things encountered in a person’s electronic health records. Like every record, an EHR needs an identification to help clinical staff find out about the patient. These might include name, date of birth, social security number, gender, etc.
3. Health History

Along with medical data mentioned before, a person’s medical history is extremely important for doctors to know. It helps them decide the dosage, makes changes to treatment, recommends additional tests, or prescribes lifestyle changes to help manage the condition better.
Since most people in the United States would have visited a doctor at least once in their lifetime, they’re bound to have a history. For those who don’t, clinicians find out as best as possible. Health history would include things like allergies, previous diseases, injuries, or major accidents (if any), in addition to the treatments administered, specific medication consumed, mental illness (if any), and so on. Such information is important because people with a certain medical history might react differently to a certain drug than people who don’t have a similar history.
People with a history of heart disease and who take medication for it would react differently to some treatments, but not people with a clean medical history.
4. Family History

Numerous diseases may be passed across successive generations. Some of those might be benign, but a few might be serious. In addition to the disease itself, some conditions present in one generation increase the likelihood of the next generation getting it. A good example of a family history of disease likely to affect future generations is cancer. Hollywood icon Angelina Jolie famously had her ovaries and fallopian tubules removed surgically, in addition to having had a double mastectomy. She took the unusual step as her family history sharply increased her risk of contracting the disease.
Another disease on which family history impacts health is Type 2 diabetes. Research suggests that people with a family history of Type 2 diabetes are between 2 and 6 times more likely to get it than people without a family history of the disease. In other words, family history of disease is an important component of a person’s electronic health record. It helps doctors manage certain diseases better and make appropriate recommendations to their patients.
5. Test Results

It goes without saying if a person’s medical history is vital for treatment, then the results of previous tests shed light on health conditions in the past. Medical histories are determined by examining blood and radiology reports from past consultations and treatments. These include X-rays, PET scans, MRIs, and CT scans and are essential in every person’s electronic health records.
6. Previous Treatments

Another vital aspect of an electronic health record is the history of treatments undergone throughout the person’s life. Looking at this gives a clear picture of what a patient has undergone in the past and helps doctors navigate their care better. Moreover, it also highlights how a particular patient responded to certain treatments, which also reveals a bit more about their conditions.
Some examples of information in this part of an EHR include data about surgeries, implants, transplants, examinations, therapy for mental health problems, vitals after treatment, and so forth.
7. Physician Notes

It’s common for physicians to make notes during the treatment or immediately after if any new information might pop up. These would be quite common for patients who have undergone extensive surgery or undergoing treatment for chronic diseases. Physicians would note patients’ responses to treatments and update the same in EHRs. Examples of these include changes in food and water consumption, sleep cycle, mental health, mood swings, vital signs, etc.
8. Financial Information

The complexity of healthcare in the United States makes it crucial for people to have insurance coverage. Without it, only the wealthiest would be able to afford anything more than basic care. So, when a patient comes in, his or her financial information is perhaps among the first details to be assessed by the clinical staff. The payer verified the insurance information to check if the treatments were covered. Only after verification is complete does the treatment begin.
This section of an EHR would include details like name, policy ID number, address and phone number of the payer, the contact information of policyholder, dependents, the relationship of the patient to the policyholder, contact details of responsible persons, occupation, the contact information of the employer, and employer of the policyholder.
9. Consent Forms

Doctors are bound by law to inform patients about the treatments they’re going to undergo. They’re also obliged to explain the details of any medical procedure and medication to the patients. Based on this information, a patient can be better involved in their care by making informed decisions.
Information in consent forms include –
- Disease/disorder diagnosed
- Recommended course of treatment
- Risks involved in the treatment
- Benefits of the treatment
- Potential and known side effects
- Chances to make a full recovery
- Risks in not taking the treatment
- Probability of success
5.Best EHR Solutions
There are a considerable number of EHRs developed by various companies. It is important to know a bit about them before choosing one to integrate with your hospital or clinic’s billing system. This section explores some of the best EHRs and their features.

It is natural to wonder which EHR would be the best to integrate with your organization’s billing system. With numerous companies offering a wide range of solutions designed for varying care settings, it is important to take a closer look at each one before deciding. Let’s look at some of the most popular EHRs that can be integrated with healthcare billing solutions –
a. iPatientCare EHR

There are two versions available for the iPatientCare EHR solution. There’s a cloud version that lets you store patient information securely on the cloud, in compliance with HIPAA. This version would require minimal investment in hardware and offers protection against loss of data in the event of any disaster. The backups, too, are stored securely to ensure business continuity.
There’s also an on-premises version available if you’re looking to invest in additional hardware and servers. iPatientCare allows its users to modify workflows to suit their own needs and can be scaled to cater to the needs of organizations of all sizes.
iPatientCare can integrate with practice management systems, hospital management systems, and other medical platforms. Moreover, it can also connect with testing centres, pharmacies, and different registries.
b. AdvancedMD EHR
This EHR solution comes with numerous features and can integrate with hospital systems, pharmacy platforms, and laboratory solutions. AdvancedMD EHR makes it easy to share information between organizations seamlessly and helps speed up the entire care delivery process. It also includes an intuitive interface.
Being loaded with features, it is to be expected that it’s going to be pricey. But it’s worth it. However, the staff at the organization will need the training to use the AdvancedMD EHR, which would also cost some more. Moreover, there is an initial price for setting it up. Although all of this makes it seem rather expensive, experts argue that its range of features makes it worth every dollar.
c. ADSC EHR
Advanced-Data Systems Corporation, ADSC’s EHR, is a cloud-based solution with many features. It includes a voice-navigation function along with a feature to recognize handwriting. These features improve the interface of the ADSC EHR and make it convenient for users.
This EHR is web-based and so accessible from tablets. Doctors and medical staff at ambulatory care centres and larger hospitals would have an easier time with the ADSC EHR as they could keep moving while accessing patient records. Meanwhile, the patients too can access patient portals using their smartphones.
It wouldn’t be wrong to say that paying for the ADSC EHR is more of an investment rather than an expense.
d. Kareo Clinical
Kareo Clinical EHR features a user-friendly interface and integrates with billing solutions, appointment scheduling software, and other third-party healthcare applications. Moreover, Kareo’s platform also includes smart healthcare analytics that shows performance metrics to help clinicians have a complete view of the business and administrative side of operations. Built especially for small practices, it is cost-effective and easy to get used to, meaning that doctors and staff don’t need to spend time on training. Furthermore, what little training is needed for getting accustomed is also provided by Kareo Clinical at no extra cost.
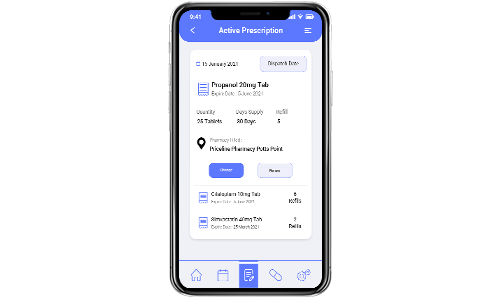
When it comes to patients, Kareo Clinical doesn’t disappoint. Its EHR platform also incorporates a patient portal to log in and view their health information. Moreover, patients can also check their appointment and prescription from their smartphones. Patients who have doubts about their prescription or anything their doctor said could use the video-conferencing feature to have a virtual consultation. Kareo Clinical’s EHR is one of the most popular for small practices, with its features and pricing, not to mention the convenience it offers patients.
e. CareCloud Chart
CareCloud Chart’s EHR solution features a user-friendly interface with a pricing model according to the support required by the healthcare organization. It means that relatively new teams would need more support, and those with experience would need lesser. Both of them would be priced according to their requirements.
This EHR is suitable for small single-physician practices and larger ambulatory care centers. It offers real-time data on patients in the form of a dashboard coupled with smart reporting, which gives clinicians a complete picture of their practice’s administrative and financial aspects. Additionally, a patient portal speeds up the process of check-in with online forms for patients to fill out before they come down for the consultation. CareCloud Chart EHR makes it a great choice for small practices and larger hospitals. It offers a good balance between cost and functionality.
6.Barriers in EHR Implementation in Medical Billing
Transformation of paper-based health data systems to digital EHR is revolutionary in every sense. But implementation of EHR in medical billing is not easy as it sounds. In this section, we are going to learn the common challenges in EHR implementation.
I. Lack of billing-friendly EHRs:
If you think a regular EHR system can handle medical billing tasks, you need to think again. Most providers today end up integrating EHR with billing without understanding the capability of their system. Even if you integrate your existing EHR system with billing, the strength of the whole system will be limited. So, it’s a wise decision to implement a billing-friendly EHR. It simplifies your billing tasks without hindering other patient history data. However, this challenge doesn’t end here. A billing-friendly EHR can turn out costly, which again is a barrier. It requires healthcare providers and developers to make strategic plans to control the cost.
II. Data Migration:
In today’s healthcare industry, the real wealth is data. And if data is mishandled, misused, or lost, it can cost billions of dollars. In medical billing software, these data are critically important. Moreover, the transition from existing software to a new one often results in data loss. Hence, data migration is required to smoothly share medical history, improve healthcare interoperability, or electronic data interchange. With smoother data migration, medical billing becomes easy and incurs lesser errors.
III. Staff Training:

Another major barrier that impacts the EHR implementation in billing is staff training. It’s just as important as other aspects of integrating EHR in billing. Since not every staff is tech-savvy, providers must help staff understand different aspects of EMR and EHR in medical billing. Besides, trained staff reduces errors and increases productivity. Thus, training employees about EHR implementation in billing is crucial. Also, providers should ensure seamless communication between employees to keep track of errors.
IV. High Cost:

The increasing cost of EHR implementation is a critical barrier. Let alone be the cost of software, training employees, and additional resources also contribute to the overall expense. Sometimes, providers incur unnecessary expenses like system failure or privacy issues, which require immediate action. Hence, healthcare providers need to plan the electronic health record (EHR) implementation to keep track of costs.
V. Privacy:

In any healthcare software product development, privacy concerns impact the care delivery and patient experience. Medical billing and coding software applications are prone to errors and privacy issues. With the implementation of EHR in billing, providers must also ensure the safety of the medical data.
vi. Lack of usability:
One of the most common barriers to implementing EHR in medical billing that the assumption that one size fits all. Typically, a medical billing staff understands the size of workflows, and if the EHR system isn’t fit, it could be a major issue. Besides, flaws in the design or poor training can also affect the billing workflows and lead to errors.
vii. Lack of communication:
In EHR implementation in billing, it’s essential to establish transparent communication between healthcare providers, patients, and IT vendors. This will ensure that the expectations of all these stakeholders are met. Since medical billing is a complicated task, the concerns and feedback of healthcare organizations/providers are important. And it’s the responsibility of the vendor to cater to it effectively. Lack of communication is the only roadblock in the successful implementation of EHR in medical billing systems.
7.Important Features to Watch Out For in EHR Billing
There is no shortage of EHR solutions to integrate with billing platforms in healthcare. Companies make EHRs for small and large hospitals, and different ones offer different features. This section talks about the most important features that are must-haves for any EHR.
It is important to know some of the important features EHRs ought to have to get a clear picture of the landscape. With numerous companies offering solutions with varying features, it might get difficult for healthcare administrators and clinicians to make an informed decision about paying for one. Let’s talks about some of the most important features that EHRs must have –
1. Reporting

This is one of the most helpful features that would allow providers to get a complete picture of the financial side of their operations. The reports display information about healthcare payments and billing submissions to highlight patterns medical professionals can bank on and make informed decisions. The data must highlight payment patterns of all patients over some time and must also include information about the insurance payers.
Information on the amount of revenue received through co-payments or out-of-pocket expenses and the time taken for reimbursements empower clinicians to better manage their organizations. Moreover, administrators at larger hospitals could have a 360-degree view of their finances and find out where they can make improvements. These would help optimize workflows and also boost revenues.
2. Assessment of Rejected Claims

Submission of claims is one of the most important aspects of the operations at any healthcare organization. It is an elaborate process that tells payers about all the treatments and procedures that the patient has received. It is prone to mistakes by its nature, and claims that are rejected would cost the provider precious revenue.
If a solution can analyze rejected claims, it will tell providers what they need to watch out for and avoid rejections. A claim could be rejected if the service wasn’t covered or if there’s a problem with the patient information, incorrect insurance details, etc. This feature would go a long way in retrieving lost revenues for providers.
3. E-Submission
Submitting medical claims is an elaborate procedure, as mentioned earlier. The larger the size of the medical organization, the more the volume of submissions handled. This will result in a few errors while filling out the necessary details and medical coding.
But EHR solutions that digitize the process make it a lot faster and introduce functions to automatically check the submissions before they’re submitted. In this way, if an EHR integrated with a billing platform features electronic submissions, it would streamline the entire process and optimize its workflows. The result is that fewer staff can do more with minimal mistakes, reducing overhead and improved revenues.
4. Rapid Verification of Eligibility
Every patient that comes in for consultation has his or her insurance coverage verified, and it ensures that the payers will cover the services rendered by the providers. But verifying health plans is a tedious process that involves considerable time and resources on the provider’s part.
But if a billing platform that can integrate with an EHR and enable fast, electronic verification of health plans would save a lot of time and staffing requirements for providers. As the verification would be faster, it would also reduce waiting times for patients who might be in urgent need of treatment. Subsequently, it results in a win-win situation for providers, payers, and the patients. The providers won’t have to worry about covered treatments, thereby ensuring timely reimbursements.
5. Payment Tracking
Being able to monitor the payment situation is an important tool for efficient operations at healthcare organizations. An EHR solution integrated with a billing platform must feature tracking of payments, and it should show when a bill has been submitted, its stage of being processed, and if payment has been made. Such functionality helps healthcare organizations know when they will be reimbursed, which engenders better deployment of resources and financial management.
6. Automated Code Transcribing

Many billing errors can be attributed to human errors in which diagnosis and billing codes are transcribed from the consultation or other medical procedures. But if this process can be automated to any extent – if patient information, codes for billing, and diagnosis can be directly incorporated into the billing documentation – then the chances of human errors are reduced significantly. This would prevent delays and denials and ensure that providers get reimbursed on time. Moreover, it brings greater efficiency and reduces staffing needs, improving revenues.
7. Copayment integrated into Scheduling
Copayments are quite common in the healthcare setting. Several patients aren’t fully covered by insurance and have to pay a certain amount as a copayment at the time of billing. And this copayment amount not only goes to the insurance companies, but a portion of it even goes to the healthcare practice. So, if a scheduling feature is added to remind the staff to collect this copayment amount, there is less chance of this amount being missed. This feature in the medical billing integrated with electronic health records can benefit the practice, as it will help increase the ROI.
8. Benefits of EHR in Billing Integrations
It is not a mystery that medical billing can be challenging for healthcare organizations. The small little things that need to be done make the entire process inherently complicated and prone to errors, affecting revenues. In this section, we discuss the benefits of adding EHR billing integrations.

The entire process of medical billing involves multiple steps that require dedicated staff. Coding, filling out claims, tracking bills, managing denials are demanding by nature. But if this process can be sped up and optimized to avoid denials, it makes everything convenient for the providers, payers, and the patients. It can be achieved through the integration of EHR with billing platforms. Let’s talk about some of the benefits that this offers –
a. Better Reimbursement

Studies and research have indicated that hospitals in the United States lose over $250 billion in revenues every year because of denied and rejected claims. The main reasons for either of these two to happen are errors in coding, errors in filing claim forms, and missed deadlines to submit claims. There are multiple reasons why these mistakes happen first, and the main one is the human element.
The elaborate procedure involves multiple steps, increasing the chances of mistakes as the number of patients increases. But EHR billing integration helps avoid all of the possibilities for errors. Bringing a consolidated digital interface to the whole process makes things easier for the staff as they can do many things with some clicks. It helps improve efficiency by –
- Notifying the staff automatically about approaching deadlines for submission
- Streamlining medical documentation and coding
- Leveraging pre-filled patient data to save time efforts for staff
These features improve productivity and minimize chances of errors, thereby ensuring that providers are reimbursed without delays.
b. Reduction in Paperwork

Medical billing invariably involves paperwork. All the elaborate processes of filling out claims, tracking their status, coding, and so forth involve documentation which the staff must deal with. However, an integrated platform would greatly reduce the paperwork and, in doing so, speed up the whole process. The advantage of reducing paperwork is the improvement in the staff’s productivity. They can get more things done with far fewer errors, impacting providers’ revenues.
c. Smarter Analytics

Just about every industry uses analytics to know where it loses money and the areas where it can make improvements. It’s no different for healthcare. Whether it’s a single-physician practice or a large hospital, analytics is known to help bolster efficiency productivity reduce losses due to various reasons.
Using EHR billing integrations, it is possible to generate detailed reports of the entire care delivery process and subsequent billing. These can be assessed using healthcare analytics solutions to discern actionable insights into day-to-day operations. This knowledge helps identify problem areas and shows where improvements would help optimize everything. The results of having effective analytics include better patient experience and improvement in provider revenues.
d. Efficient Interoperability

EHR billing integrations are known to have a high degree of healthcare interoperability. The healthcare information within this system can be shared with multiple medical professionals to engender a collaborative approach to care and improve clinical outcomes for patients. A major advantage of EHR billing integration is better managing all the patients’ data. Since the data is in a central repository, it can be accessed by staff to help speed up the process of filling out claims and other non-medical workflows. The benefit of a centralized system of managing all the information allows for better security measures to be implemented. This, in turn, also makes it easy to adhere to prevailing regulations.
e. Superior Patient Experience

Most patients often find the whole experience with healthcare payments rather stressful, which flies in the face of ensuring patient satisfaction. An EHR integrated medical billing system would accelerate verifying the insurance plans of patients and reduce the waiting times before physicians can begin treatments.
Patients would also find out if they faced unexpected costs through an EHR integrated billing platform through their providers. Knowing exactly which the payer covers medical services makes things convenient for both the providers and patients, who can ensure that they won’t face unforeseen expenses—the result in a definite improvement in the overall patient experience with the provider.
f. Optimized Billing Workflows
Without an integrated billing system, the entire medical billing procedure is bound to get highly inefficient. An EHR integrated billing solution reduces the sheer amount of paperwork and speeds up the entire process by automating many parts of it. Doing so reduces the chances of human error and that of claims being rejected or denied.
The increase in productivity and reduction in mistakes leads to lower overhead and better revenues for providers.
g. Reduced Accounts Receivables

Rejected or denied claims result in major dents in the revenues of healthcare organizations. This affects the providers and the patients since the quality of care is likely to decrease as the revenues plunge. An EHR integrated billing platform enables fast and accurate verification and coding, not to mention tracking and monitoring claims status. These factors go a long way in reducing the accounts receivables and ensuring that providers get reimbursed on time.
h. Improved Staff Productivity

An EHR integrated billing solution automates many aspects of the medical billing workflow. Things that used to require lots of paperwork can be done with some clicks, and the staff doesn’t have to deal with as much documentation. Consequently, there are far fewer errors in billing, which leads to better revenues for providers, as mentioned earlier. In other words, the same number of staff can do more with greater efficiency without errors. It is safe to say that an EHR integrated billing solution maximizes the staff’s productivity.
i. Increases accessibility to Medical Bills
Online EHRs run on a single server in the healthcare organization or practitioner’s office. However, customized EHRs are accessible from anywhere with an internet connection. That means, with EHR-integrated medical billing software, the provider can have accessibility from anywhere, anytime. And if it’s a mobile application, it becomes even more convenient to access medical billing records anywhere.
j. Brings Transparency between provider and patients
As integrated EHR systems offer more transparency between patients and providers, their integration into medical billing solutions will also provide a similar benefit. With EHR in billing, providers and patients can easily access payment information. Patients will feel they aren’t charged unnecessarily, and providers can retain patients. And this will ensure better communication and build trust between providers and patients, ultimately boosting patient experience and satisfaction.
9. Can Mobile EHR Software Improve Medical Billing?
We’ve talked about all the benefits of EHR integrated billing solutions and how it helps providers. This section will discuss the steps to integrate EHRs with a billing platform within a reasonable budget.
Healthcare organizations understand the power of mobile EHR systems. From convenience to flexibility, these EHR/EMR systems have empowered clinical staff to access patient information and handle records from anywhere. They no longer need to be near their desktops systems to transfer physicians’ or patients’ health records or even manage different tasks.
Even in medical billing, mobile electronic health records can assure more flexibility. This trend will inevitably grow further in the coming years. Take a look at how mobile EHR can improve medical billing-
- Desktop systems are outdated: A dedicated mobile EHR app is much better than traditional desktops. Flexibility isn’t the only benefit, but with mobile applications, entering data also becomes easy. It’s not like the desktop version is fitted into the mobile, but such an application is specifically built by developers considering the smartphone or tablet’s capabilities. And with mobile EHR integrated with medical billing, administrative staff feel more relaxed. They can easily update the billing and other payment details directly on the mobile apps, no matter where they are. And if they need to share billing information with patients while they are on the go, mobile applications give them an upper hand in that too.
- Offers more convenience and speed: As mentioned earlier, mobile EHR apps are the perfect example of having convenience at your fingertips. There are times when doctors are busy outside their offices or on leaves. And on an emergency call, they need patient data. Should they go to their desktop systems or make the patient wait? Well, that’s not required because mobile EHR offers the convenience and required speed to access patient data whenever required. Also, doctors can update patients’ conditions on the electronic health record systems during care episodes through mobile applications without touching their desktops. This advantage also applies when it comes to medical billing.
- Security is Crucial: Patient records are most prone to cyber-attacks making HIPAA compliance a must. Developers ensure this for the EHR software particularly. Ensuring all security provisions for EHR software is essential because the records are often shared across healthcare organizations, patients, insurance companies, pharmacies, etc. Security breaches and data loss are high risks, costing providers millions of dollars. The same applies to mobile electronic health records. Today’s developers ensure higher security in mobile EHR systems through robust encryption and other privacy protection techniques to ensure the safety of patient health information. And in EHR integrated billing, this can benefit the provider immensely.
- Benefits Administrative Staff: Administrative staff tends to benefit the most from mobile EHRs. Typically, EHR software integrated with ICD codes makes the data entry process in the patient’s charts faster and easier. Even the billing process becomes more efficient. Indeed, the healthcare practices’ specific templates also make it simple to add the correct information at the right place with minimum effort. This ensures an errorless data entry before the staff moves on to the next page. Doing this on a mobile application is even easier, as the staff can do it anywhere.
So, it’s quite right that mobile EHR will make medical billing even more convenient, less time-consuming, and more flexible.
Conclusion
Medical billing is prone to delays and mistakes that directly or indirectly affect providers and patients alike. But an EHR integrated billing solution can iron out all the kinks in the workflows of medical billing and, in the process, help the patients, providers, as well as the payers themselves. In other words, it has become an indispensable part of the healthcare industry, and the more providers adopt it, the better it will be for all stakeholders involved.
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.