Table of Contents
Patient portals, patient engagement systems, advanced telehealth solutions, remote health monitoring systems, and EMR systems are some of the most prevalent digitally powered healthcare systems. And all these applications’ interoperability ensures a seamless flow of information and connects the entire health system. And the interconnectivity of these solutions with the EHR system is most important considering its potential. However, connecting one solution with electronic health records software and guiding a successful system rollout is difficult. That simply indicates the lack of EHR interoperability.
Today, medical practices acknowledge the importance and value of interoperability solutions in healthcare. And they’re rapidly adopting these interoperability solutions, especially EHR interoperability solutions. By 2025, the worldwide digital healthcare market is expected to reach $500 billion. And according to MarketsandMarkets reports, the global market for healthcare interoperability solutions is predicted to reach 4.2 billion USD by 2024, going up from 2.3 billion USD in 2019. Even with all the advantages, EHR interoperability in healthcare is difficult to implement. Health-tech professionals are struggling to manage PHI and the variety of EHR systems. Furthermore, some people are concerned about personal information privacy and data systems’ security. So, data protection and confidentiality are ensured by leveraging new and more secure technologies such as healthcare cloud computing or Blockchain.
Besides that, this article will focus on EHR interoperability solutions and highlight the need and scope of this solution in today’s clinical ecosystem. Also, we’ll shed light on how to improve and measure EHR interoperability technology solutions about the current standards and frameworks. Perhaps, before we dive into that, it’s essential to understand the role of interoperability in healthcare and its usage levels in the healthcare landscape.
What does Healthcare Interoperability Imply?

Healthcare data has always been difficult to capture, manage and exchange securely across different platforms and clinicians. Well, the nature of health data creates a paradox: it’s difficult to share because it’s sensitive and requires high privacy and security. But being unable to access it when needed most generally leads to considerable harm for patients and providers. The lack of healthcare interoperability can lead to an incompetent understanding of an individual’s or population’s health needs. And this leads to negative clinical outcomes and higher expenses.
Interoperability solution has been a hot topic in healthcare for over a decade. The passage of the HITECH Act in 2009 marked a watershed moment in which healthcare staff was strongly urged to adopt EHR instead of paper-based records. And with increased EHR usage, secure data transmission became a big concern owing to the lack of interoperability between healthcare solutions.
Well, interoperability is most simply defined as the ability of the software, information systems, and devices to link and integrate within and outside the limits of the healthcare organization; to ease access and exchange of patient data to address health challenges in general. Further, interoperability and data exchange today is increasingly important for delivering effective healthcare, as populations worldwide are aging and people want to live longer. The Agency for Healthcare Research and Quality estimates that two out of every three older Americans in the United States have at least two chronic behavioral or physical illnesses. And treatment for such patients with numerous chronic illnesses currently accounts for around 66% of all healthcare costs in the United States.
According to the Office of the National Coordinator for Health Information Technology (ONC), the use of electronic health records has expanded considerably in the United States. Even though many hospitals now routinely receive medical records and patient data from external providers, less than half of hospitals integrate the data they get into individual patient records. So, it’s clear that access to critical clinical data has increased, but much more effort is required to bring stakeholders together to develop an integrated data ecosystem.
Today, health data interoperability benefits companies throughout the healthcare industry. That means providing physicians and other healthcare practitioners with a complete picture of their patient’s health status or condition. Health plans could better understand utilization rates and service demand if health information systems were more interconnected. Even government service providers would be able to access demographic data to identify trends and satisfy the needs of their citizens. Furthermore, life science companies could use large databases to conduct faster and more informed research.
Thus, with improved interoperability, organizations could stop seeing individuals as patients one day, health plan members the next, and health app users after that. Instead, decision-makers across the healthcare sector would be able to begin looking at how users access and use health information, independent of its source, to create better care models, improve patient safety, and improve experiences for those they serve.
Levels of EHR Interoperability in Healthcare
According to Healthcare Information and Management Systems Society, interoperability solutions in healthcare can be categorized into four levels.
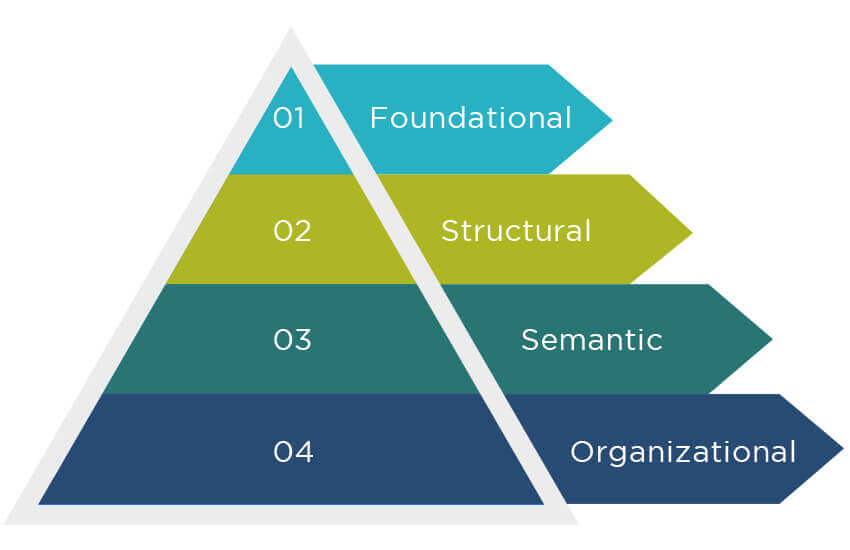
Level 1: Foundational
At the foundational (Level 1) level, health systems establish the interconnectivity standards required for one system or application to properly communicate data. Easy and seamless transfer of clinical data from a health system to a user or another platform is the lowest level of interoperability. Clinical data is securely sent from one system or device to another without being interpreted or formatted. In other words, the information shared with the user or receiver platform doesn’t need interpretation. For example, a nurse manually inserting information from a PDF file containing a patient’s most recent lab results into the patient’s health record is foundational interoperability. When a patient gets discharged from the hospital, the health summary they get in PDF is another example of foundational interoperability, as this document doesn’t need any interpretation.
Level 2: Structural
Structural interoperability in healthcare is the ability that specifies the organization and formatting of data transfer, which also includes how data fields are interpreted. When structural interoperability, or structured transmission, is established, all data is standardized to a precise format so diverse systems or devices may interpret it. Further, this data is organized in a certain manner to allow the receiving system to automatically detect specific data fields. Due to the structural interoperability provided by data standards like FHIR and HL7, medical records can be consistent, aggregated, and readily moved between systems. Besides, both the sending and receiving systems must follow the accepted data standards to ensure structural interoperability. The perfect example of this level of interoperability can be seen in e-prescriptions.
Level 3: Semantic
Semantic interoperability is the ability to provide for common models and codification of data that allows the usage of data elements with well-defined meanings from widely accessible value sets and coding vocabularies, offering users a shared understanding and meaning. Besides, data interchange across systems with radically different data structures occurs at the semantic level of interoperability, sometimes called ‘semantic transport.’ Imaging systems, which handle several specialized DICOM and non-DICOM picture formats, give an obvious example of semantic interoperability. Further, semantic interoperability allows images to be transferred, interpreted, and incorporated between multiple systems regardless of their original format or source. However, as systems offer the same information in various ways, determining what data to acquire and convey can be difficult. As a result, some experts believe that artificial intelligence will be required to achieve comprehensive semantic interoperability. Further, semantic interoperability allows providers to share patient health data with other healthcare providers using different EHR software.
Level 4: Organizational
This level of interoperability, appended in March 2019, is popular in the healthcare landscape. Organizational or Level 4 interoperability factors include governance, policy, social, legal, and administrative issues to facilitate safe, frictionless, and timely data exchange and utilization within and between companies, entities, and people. These components enable integrated, shared, and trust-based end-user procedures and workflows. So, organizational interoperability refers to the seamless data flow between multiple organizations with different criteria, policies, and goals. At this level of interoperability, governance, policy, and technology innovations ensure integrated workflows, security, and consent among a diverse set of healthcare stakeholders. Perhaps, other experts believe that organizational interoperability, rather than semantic interoperability, is the highest level in healthcare.
Scope of EHR Interoperability Solutions
According to Research and Markets report, the projected value of the healthcare interoperability solutions market by 2026 is estimated to be $5.7 billion. Despite multiple challenges, EHR interoperability is rapidly expanding, and some experts believe that EHR/EMR interoperability will get more advanced in the next few years. According to a study conducted by Deloitte, 80 out of 100 technology executives have revealed that they have hired data architects to define their interoperability strategies. This indicates that the scope of EHR interoperability technology solutions is flourishing.
As per the principles of EHR interoperability, all patient data, including health and well-being information, will be interconnected and available for action and research. Another Deloitte report reveals that health data streams will converge by 2040, resulting in a highly tailored and comprehensive view of each patient’s health. This shows that EHR interoperability will leverage clinical decision-making and boost patient outcomes.
So, the scope of EHR interoperability solutions includes:
1. Integration
EHR interoperability solutions aim to integrate internal data, processes, and users to ensure the data is actionable. The integration will expand the scope of EHR interoperability, enabling different systems, such as practice management solutions, LIS, and more, to seamlessly communicate and share data efficiently. Besides, the integration will benefit healthcare providers and practices immensely. Providers can comprehensively view patient medical history, test results, and treatment plans. And from this information, they can draw insights, identify patterns, and ensure better coordination and collaboration with other healthcare professionals, if required. Further, the integration in EHR interoperability improves the efficiency of workflows, minimizes duplicative efforts, and boosts patient outcomes while making the data easily accessible across different systems.
2. Exchange
Apart from integration, exchanging data or patient health information also highlights the scope of EHR interoperability solutions. It enables providers to timely share or exchange health data. Since health data is often shared among care professionals for different purposes, the timely exchange can prevent many mishaps. For example, on-time data sharing can save patients’ lives or detect acute diseases early. So, EHR interoperability facilitates the secure sharing of sensitive patient health information across hospitals, clinics, and pharmacies. Besides that, EHR interoperability solutions enable seamless data exchange, support early disease detection, improve coordination of care, and enhance patient safety. Take, for instance, if a patient visits a new hospital or emergency clinic, providers get access to their complete medical history can allow them to make informed decisions quickly and deliver accurate and rapid care.
3. Access

EHR interoperability solutions attempt to make data access easier and more secure for healthcare professionals, patients, and other authorized entities. Besides, interoperability solutions also improve service quality, patient outcomes, and the overall customer experience by ensuring the proper people can access patient information. With patients benefiting from access to their health information, EHR interoperability allows them to actively participate in their care, make informed decisions, and collaborate with their healthcare professionals on shared decision-making. Furthermore, interoperability solutions enable the secure interchange of data with third-party apps, allowing for the development of innovative tools and services to improve patient involvement and individualized healthcare delivery. And not just third-party apps but clinical trial companies as well. Having access to patient health data, these clinical investigators and CROs facilitate clinical research for drug development, precision medicine, etc. Hence, accessibility factors seem as crucial as exchanging patient health information.
4. Insights
To draw meaningful and actionable insights, EHR interoperability solutions use health data from clinical records, claims data, and device monitoring data. These solutions also capture data from social determinants of health, including financial, housing, and economic elements, for insights. Besides, interoperability solutions in healthcare can enhance population health management, uncover patterns and trends, and enable evidence-based decision-making by collecting and analyzing these disparate data sources. In short, the insights collected from various sources are used for these purposes. Healthcare organizations, for example, can identify high-risk patient populations, track disease outbreaks, and devise targeted therapies and preventive measures by analyzing massive databases. These insights contribute to better healthcare delivery, more effective resource allocation, and better health outcomes for individuals and communities.
8 Major Barriers to EHR Interoperability
Since EHR interoperability is only achieved by integrating disparate electronic health records or EMR systems and ensuring the accessibility of health data both internally and externally of the health system, well, it won’t be wrong to point out that the current goal of the US Health and Human Service Department is to achieve plug-and-play EHR interoperability. Also, the HHS demands the EHR interoperable ecosystem by 2024 must deliver correct data on time to specific users across health systems, organizations, and people.
Multiple technical and administrative barriers may be involved in integrating and implementing EHR interoperability solutions. The core barriers today are:
1. Consistency and Homogeneity

According to Erich Senin Huang- “The lack of a cohesive data model for patients in most electronic health records — an intuitively patient-centric construct that allows clinicians to start with a patient and trace back to their signs, symptoms, and diagnostic tests.”
Several experts have assessed and analyzed the EHR software solutions’ readiness to handle the pandemic crisis of today. And they arrived at some disturbing conclusions. A key point these experts noted was the lack of homogeneity in all major EHR solutions. The lack of homogeneity in EHRs can lead to many complications, hampering clinicians’ work.
Further, inconsistent network data is another barrier to EHR interoperability solutions. Clinicians or administrative staff often suffer a lot due to this inconsistent data. Storing different pieces of information in disparate places, not at a centralized location, clinical staff have to waste countless hours searching for specific information when needed. So, adopting a single or central unified network and interface, automatically drawing out the required data from disparate silos and, thus, developing a uniform dataset can make a lot of difference. That means such networks and interfaces can guarantee smooth and seamless workflows.
2. Unified Patient Identification

Another barrier to EHR interoperability in healthcare is the lack of unified patient identification. Typically, this issue is mainly due to the lack of patient identification standards, which are accepted nationwide (NIPD). NIPD helps in patient matching, leading to a minimized rate of repeated tests and delays in care incidents. Besides that, a unified patient identification number (UPI) empowers healthcare companies to tackle critical EHR and EMR issues such as duplicate entries and overlays. Well, these are quite common reasons behind the problem of patient misidentification.
A proper UPI can save healthcare practices and clinicians from other major problems. Patient misidentification usually results in grave consequences and discrepancies, including repeated tests or procedures, erroneous prescriptions, and extra costs. So, it’s the job of clinical staff to ensure the correct patient identification. And that would ultimately resolve this barrier to interoperability in EHR.
3. Data Sharing Among Payers

Insurance companies have to deal with loads of different patient data. But they’re often hesitant to share it with healthcare providers. With the value-based care model in place, providers and payers need to share data to operate efficiently. And with a common goal in mind, which is reducing the cost of care without compromising patient care.
As a result, payers require access to clinical information or the important insights provided by data. And at the same time, providers also want information on patients’ demographics and social determinants that payer companies record and store. A clear understanding of the common purpose enables payers and healthcare providers to accept mutual data sharing, ultimately resolving the roadblock to interoperability.
4. Integration Costs
To guarantee high-quality care, clinicians use various health information technology systems, from EHR to other automated healthcare solutions and analytics tools. Perhaps, these disparate systems should be seamlessly integrated.
The catch is that many providers often believe integrating health IT systems, particularly EHR, is an expensive investment. And think that such integrations only large healthcare networks can afford. At the same time, when IT vendors build healthcare systems, they often integrate them into the hospital’s IT infrastructure. Due to these misconceptions, integration costs are a barrier to healthcare interoperability solutions.
5. Updates and Scalability
Enabling providers to track patient health records is what EHRs are pro at. But most EHRs are complicated, with numerous interconnected functions, making trouble-free updating and scaling nearly impossible. This is a lengthy and costly process for providers. During the pandemic, some Duke University researchers discovered that modern EHR systems could not serve as population health management software. Only expert IT vendors can build EHR with multiple capabilities and ensure timely updates.
6. Resistance to Data Sharing

Despite the increasing importance of interoperability and data-driven care models, certain healthcare providers resist sharing data with their peers. For example, if hospitals are competing with urgent care clinics for patients, they will have little interest in exchanging patient data when the request comes from emergency departments.
On the other hand, health data must be accessible and available across organizational boundaries. According to the Cures Act Final Rule issued by the ONC, healthcare stakeholders must implement standardized APIs that allow individuals and healthcare providers to securely access structured electronic health information through mobile applications. And if the data is not available, the provider can be punished and labeled a data blocker. This highlights how resistance to data sharing can be a major obstacle in healthcare interoperability solutions.
7. Cross-EHR Communication

Fast Healthcare Interoperability Resources (FHIR) has quickly become a standard protocol for integrating various healthcare-related systems to assure cross-EHR connectivity. Besides, it is a “data transport layer” that typically boosts interoperability in healthcare. Today, while most providers use FHIR, the lack of strict requirements makes seamless data sharing difficult.
The real issue with the FHIR and data sharing is that FHIR defines over 150 resources. These resources include even the smallest feasible units of relevant data. But most healthcare organizations only use a subset of them, which is considered incorrect. Since the fundamental FHIR principles are interrelated, healthcare practices using this narrow selection tend to jeopardize interoperability altogether. So, to achieve seamless FHIR interoperability, providers must first create a set of components and resources they require. After all, ensuring FHIR is quite critical for EHR interoperability.
8. Patient Data Security

Patient data security can be a significant issue for EHRs. Providers should implement protections under the HIPAA Security Rule and other applicable requirements to ensure seamless and secure data transmission. This is not new to providers, as all healthcare practices, clinics, and other entities must comply with HIPAA regulations.
The technological systems that access ePHI (electronically protected health information) must be subjected to technical protections. Healthcare organizations must implement a system for encrypting and decrypting electronic protected health information. They should also implement transmission security measures to prevent unwanted access to ePHI while it is being transmitted. Only by taking all these measures, from full compliance to regulatory protocols, can providers reduce the cases of cyberattacks and security breaches and ensure patient data security. Indeed, patient data security can even promote and boost the ability of EHR interoperability in healthcare.
How to Improve EHR Interoperability
From these 8 barriers, it’s evident that EHR interoperability needs some improvements. Addressing cost, consistency, security, and scalability issues is primary. As already mentioned, these barriers are stagnating the capabilities of EHR, and providers fail to achieve interoperability. To ensure interoperability, providers must consider specific technologies and strategies to overcome these barriers. And facilitate a seamless data flow across different health systems, organizations, and entities. Besides, some experts believe that cloud computing and Blockchain effectively enable full-scale interoperability and overcome other communication roadblocks.
Well, leveraging these two technologies in EHR software can assure interoperability, and here’s how-
1. Adopting Cloud Technology

EHR cloud migration is in high demand right now. Cloud EHR deployment reduces the hefty costs that healthcare providers must suffer by providing a pay-as-you-go strategy. Furthermore, the cloud environment helps healthcare providers to alleviate some of the security load. Most cloud EHR companies provide round-the-clock support and specialized cybersecurity services to keep PHI secure. Besides, data sources like clinical, lab, and pharmacy systems can readily integrate and access cloud-based EHRs. This guarantees interoperability across all health systems and entities and enhances the quality of patient care.
Moreover, cloud-based EHRs allow consumers to store their data on several servers in different geographical regions. This makes it simple for users to save and retrieve data as needed. It also includes advanced security features that protect data from hackers or illegal access.
These benefits, however, are limited to public and hybrid clouds. If providers create and deploy EHR on a private cloud, it could be expensive and require a professional in-house IT team.
2. Leveraging a Blockchain EHR
Blockchain technology is a decentralized, public digital ledger that permanently and verifiably records transactions. Blockchains are inherently resistant to data manipulation and are also resistant to data modification as per their design. Further, it increases EHR interoperability by allowing users/patients to share their medical records with their healthcare providers via a secure, private blockchain network as requested by the provider. Blockchain has unique security characteristics, such as creating an audit trail, in the case of malicious actors to reduce the risk of data loss.
Blockchain has the potential to improve semantic interoperability. Developing costly interfaces across different EHR systems using Blockchain is unnecessary. Just a private key is all that is required to access patient records. Also, this may allow any healthcare professional from any location to view health records with the correct credentials. Patients who use a blockchain EHR become full-fledged masters of their data, which may increase patient involvement. They provide clinicians with access to their health information, not vice versa. In this situation, consumers are on their own to combat cybercriminals and dangerous actors.
3. Healthcare APIs

The most frequent method for achieving interoperability is through open Application Programming Interfaces (APIs). Data and protected health information (PHI) can be shared and transmitted between EHRs and health information technology systems through APIs, enabling easy communication between disparate applications and health systems. Besides, APIs make internal and cross-organizational software interoperability easier for healthcare providers. They promote shorter deployment times and offer easy access to medical data, lab results, and other information for patients. As a result, FHIR APIs will be integrated into all healthcare platforms shortly. They also establish a consistent standard for all systems, simplifying third-party integrations.
4. Artificial Intelligence

Today’s fastest-growing technology Artificial Intelligence is also one of the ways to improve EHR interoperability. Thanks to machine learning capabilities in the core of AI systems, it can process large volumes of data such as patient forms, clinical notes, and health records. So, scalability issues in EHR and other data-related interoperability concerns can be easily dealt with AI technology. Additionally, AI systems integrated into EHR software offer crucial and current insights, irrespective of their data sources. These insights facilitate clinical decision-making to ensure better patient outcomes.
Now with these four ways improving EHR interoperability can get quite simple. Besides, standardizing data entry will be critical for future interoperability in medical information systems. All stakeholders should collaborate to develop a standard that makes it easier to extract patient data, providing organizations with the most up-to-date and relevant information. Another step should be to centralize this data throughout the healthcare ecosystem. Furthermore, by 2040, every contemporary medical company may be bound to embrace radical interoperability. And radical interoperability means that every individual’s unified health information will be accessible for research and therapeutic purposes so that clinical trials or CROs can directly access patient health records to leverage clinical studies.
Besides that, the relevant initiatives of the US government aim to improve coordination and management, care quality, patient safety, and outcomes. It also aims to boost patient privacy and security, staff productivity, operational effectiveness, knowledge sharing, medical research, medical error rates, healthcare costs, and complete population health. New software systems will always be required to communicate with one another. Above all, APIs will enable interoperability and other critical advancements for practices, as they want to meet patient demand for accessing medical records, shift to value-based care, and fully utilize analytics.
How to Measure EHR Interoperability
Just leveraging technical strategies to improve EHR interoperability isn’t enough. From time to time, providers must also measure EHR interoperability to understand whether it’s functioning well or not. As previously mentioned, EHR requires regular updates, which can often hinder the interoperable abilities of the software. Apart from that, there are other elements that can impact it. So, it would be quite wise for providers to take steps to measure interoperability in electronic health records.
Well, measuring interoperability is a complex process. It can be quite time-consuming and often requires extra effort from providers. Hence, providers must break a sweat if they are keen on keeping the EHR software agile and ensuring full interoperability.
Besides, before we can decipher the quality, usability, and other success metrics, we must first answer the notion of the “volume” of health information transmitted. Once we’ve agreed on the fundamental volume metric, we can move on to defining more criteria to fully comprehend the scope and impact of interoperability throughout the healthcare system. Perhaps, we acknowledge that multiple organizations are working to define these volume metrics, but they may be doing so separately and without the knowledge of the larger community. Suppose we are to progress toward a consistent understanding of how well interoperability is progressing. In that case, we must break through these silos and begin a meaningful discourse as a community to establish these measurement metrics.
The HIMSS Interoperability and HIE Committee has proposed and developed 8 measuring factors to measure interoperability. Providers can effectively measure interoperability using these factors as per their healthcare organization or health system. Also, these measures with factors will allow providers to rate the scope of interoperability with EHR and its efficiency and even identify potential gaps. Here are the 8 factors to measure to ensure seamless interoperability with EHR systems.
1. Partners and Stakeholders

This factor proposed by HIMSS highlights how data exchange is considered at individual and population levels. So, partners and stakeholders are just individuals and entities that the interoperability network of the healthcare organization supports. Typically, this may include measurement of data exchange or interoperability at the individual level. And that would be patients, providers, payers, and other authorized stakeholders or entities. Besides that, measuring data exchange at the population level will include registries, reporting, and so on.
2. Application of Standards
Message types and standards that enable the receiver to recognize and process data are included in this element. Typically, these standards are employed in the transactions. Some of the metrics in these standards proposed include:
- Capture of the message type: When a message is sent across the health system or to a user entity, the message will fall under a specific category. And these categories are identity, admission, orders, results, referral, discharge, and so on.
- Standards utilized for each: Each transaction has to follow a standard to ensure effective data exchange. And these standards to check are direct, HL7 V2, V3, FHIR®, DICOM, GS1, ISO, and other standards typically used for each transaction.
3. Basic Transactions
Basic transactions are described as the ability of two or more technologies or systems to exchange information in a fashion that the receiving system can use natively. In short, the ability of two systems to exchange data and the receiver’s ability to utilize the information efficiently. Besides, these metrics would assess the volume and kind of transactions. It is suggested that these transactions be measured as follows:
- Send
- Receive
- Query and Find
- Use and Integrate
4. Profile-defined Transactions
Profiles such as IHE, test venues, and implementation guidelines define transactions. Data collected during testing events and connections allow for the adoption of standards to be measured. Further, with this factor, providers can measure EHR interoperability across external entities.
5. Transaction Time

Another measuring factor that can be used is the transaction time. This factor determines whether the data is sent internally or outside the health system in real-time, in less than 15 minutes. If not, it’s considered delayed, or it will be sent one batch later.
6. Transaction Volume

The volume of transactions for each technology type and network-reported trend data indicate substantial rises, declines, or flatness. That means significant changes in the volume of transactions and reported data can aid in developing plans for scaling up transactions. And also determines the efficiency of interoperability across the health system.
7. User Specifics

Apart from the transaction detailing, interoperability in the data transaction is also based on the user’s characteristics. The size, location, and specialty of healthcare businesses contribute to a better understanding of the environments that host interoperable transactions. By size, it means bed size or the number of registered network users/clinicians, and location means rural or urban settings. All these combinedly determine the interoperability in transactions or data exchange.
8. Future Plans
Plans mean one to two years to expand on the types of transactions a healthcare environment intends to support. In other words, at this point, providers may devise methods for bridging gaps and progressing toward semantic interoperability with more healthcare systems, if necessary.
EHR Interoperability Framework and Standards
EHR Interoperability standards and frameworks are just a set of regulations or protocols that enable disparate EHR systems built by different developers to communicate and exchange data efficiently. EHR interoperability standards facilitate the improvement of care quality by making specific and accurate healthcare data available to the right person at the right time. That means providers can access the correct health data in no time. Despite the development of EHR interoperability standards, there is no uniform standard. Many healthcare experts still consider True EHR interoperability a work in progress.
FHIR (Fast Healthcare Interoperability Resources) is the most popular and widely accepted standard for healthcare interoperability. Other standards exist for various data types and procedures, such as DICOM for sharing medical images between systems such as picture archiving and communication systems like PACS. Further, ICD-10 employs standard codes for diagnosis and billing procedures, and HL7 V3 for exchanging demographic, clinical, and administrative data and many others. While these standards are vital, complete EHR interoperability will be impossible without a single technical standard.
Perhaps, let’s look at the current standards and frameworks of EHR interoperability:
1. Fast Healthcare Interoperability Resources

FHIR is explained in the simplest manner by Micky Tripathi, the national coordinator for health IT at the Department of Health and Human Services- “When you order something on Amazon, for example, look at your browser line; If you’re logged in, and you click on something, what you’ll see is a URL that says ‘HTTP’ and then this huge string of nonsense. That’s a query-retrieve system that’s generated in your browser and sent to Amazon, and then Amazon immediately returns the results securely.”
On the internet, people from all over the world can use any standard browser running on any web-enabled device, whether it’s a smartphone, laptop, or tablet running a Windows, Apple, Android, or Linux operating system, to visit the same URL and complete the same tasks. And FHIR hopes to do the same thing in healthcare.
HL7 International developed and maintained the Fast Healthcare Interoperability Resource, a proposed data standard. FHIR was designed with the complexity of healthcare data in mind, and it employs a modern, internet-based method to connect several distinct pieces. Besides, data elements, or “resources,” each contain a tag that serves as a unique identification, similar to a web page’s URL.
FHIR enables the transition from hospital-centric to patient-centric collaborative healthcare. And this allows physicians and patients to gain what they need from health IT systems. Besides, patients can connect with physicians in various places and healthcare settings while maintaining a single personal health record containing comprehensive data relating to all their drugs, issues, allergies, and consultations.
Apart from these, FHIR is a specification and an open, standardized web API. The FHIR API is built on well-known web standards such as XML, JSON, HTTP, OAuth, and REST. So, utilizing these popular technologies lowers the barriers to entry and makes implementation easier and faster, even for engineers with no prior healthcare IT experience. Additionally, RESTful HTTP commands are used to make FHIR queries and searches, which return drugs, observations, and patients represented as FHIR resources. An FHIR request can return a single resource. It can be a patient’s personal information, data collection, a treatment plan, and drugs, or a bulk data bundle for all patients in an EHR.
Above all, FHIR has numerous prospects, and support for the data standard is widespread across the care continuum. Providers and patients will have access to an exceptionally comprehensive range of functions within their health IT systems as FHIR continues to support data sharing.
2. Trusted Exchange Framework and Common Agreement

TEFCA, or Trusted Exchange Framework and Common Agreement, was first recommended by ONC in January 2018. It was proposed to expand and improve interoperability and enhance providers’ and patients’ capacity to securely access and utilize data from various sources. TEFCA consists of a Trusted Exchange Framework and a Common Agreement. While TEFCA is designed to promote nationwide connectivity of electronic health records, it cannot function until a network of provider organizations joins the Qualified Health Information Networks, or QHINs, which permit data sharing. Unfortunately, many suppliers are still unfamiliar with the new arrangement, according to industry experts.
Other than QHINs, HINs are another type of trusted health network. To define HINs, these networks have policies and operations to allow business associate partners to share and exchange patient health information. To better understand this, let’s take this example- HINs are ATMs, while QHINs are the cards that can be used in those ATMs.
Besides, the Common Agreement specifies the rules and conditions that apply to an RCE (Recognized Coordinating Entity). It will also define the infrastructure model and governance strategy that enables users in different networks to share fundamental clinical information securely under commonly agreed-upon expectations and norms, regardless of network. Further, QHINs will voluntarily adhere to the terms of the Common Agreement. And it’s the RCE that will make QHIN coordination and compliance with the Common Agreement a reality.
Let’s consider this example to better understand how TEFCA works. Imagine you live in Boston and have to go to Orlando for a vacation. But there you become sick or wounded. You would want your medical record to be accessible so that the doctor caring for you in Orlando has all the information he/she needs to provide you with the best quality care possible. And this is where TEFCA will benefit you.
Another example is when patients are moved from a rural care environment to a distant treatment facility. The ability to connect rural and urban care settings is an expected benefit of TEFCA. TEFCA will allow for this comprehensive and accurate understanding of a person’s medical history.
ONC also published the TEFCA FHIR Roadmap, which details how TEFCA plans to boost FHIR adoption across the healthcare industry. Furthermore, ONC understands that health data transfer is currently heavily reliant on established standards. This includes integrating the Healthcare Enterprise profiles and HL7 C-CDA. Also, on how FHIR offers a more modern method. Moreover, the road map also includes a three-year strategy to boost adoption through what ONC refers to as “achievable, incremental steps.”
Above all, healthcare leaders must stay current on TEFCA developments. It’s not only because of the already mentioned driving forces, but they should also focus on the long-term goals and positive outcomes of TEFCA participation, such as eliminating gaps in care, lowering the cost of care, and providing the best care for their patients.
3. Center for Medicare and Medicaid Services

In 2018, the Centers for Medicare and Medicaid Services, the Office of the National Coordinator for Health IT, and the White House Office of American Innovation made a public commitment to ensure that patients have access to their healthcare data wherever and whenever needed. And then CMS embarked on a journey to break down the barriers that keep critical patient health information locked in digital silos. For years, the path to healthcare interoperability has been a relay spanning numerous administrations, each passing the baton to the next. And that brought the healthcare industry closer to the objective but always fell short of seamless health data interchange.
CMS’s proposed rule of Advancing Interoperability and Improving Prior Authorization Processes, announced on December 13, expands on its 2020 Patient Access and Interoperability rule with new requirements for CMS-regulated healthcare payers. These payers would be expected to do the following under the proposed rule:
- Establish APIs to share information with care providers about those patients who fall under this plan category.
- Also, share information with other payers in case patients change their plans.
- Allow providers to collect details related to coverage requirements for items and services that need prior authorization.
- Lastly, submit information related to the authorization.
Further, CMS proposes that payers use the Health Level Seven Fast Healthcare Interoperability Resources standard for these APIs. And even for other interoperability specifications previously adopted by ONC on behalf of HHS and referenced in ONC’s Health IT Certification Program and CMS’ Patient Access and Interoperability final rule. Besides, the data and standards established in ONC’s United States Core Data for Interoperability (USCDI) are also incorporated into the set of data that CMS requires payers to make available through these APIs. So, these are critical efforts in advancing an API ecosystem built on open industry standards throughout the healthcare value chain.
Lastly, these APIs can streamline the documentation process across the entire system. And it will also enable providers to send prior authorization requests and receive replies directly from EHRs. Looking forward, we’re sure this CMS standard has already laid a solid foundation for interoperability. And it will continue to expand by examining policies that boost interoperability and minimize burdens.
4. United States Core Data for Interoperability

USCDI is a standardized set of data items that can be routinely and easily shared, including patient names and medication lists. It’s the starting point for what diverse health-tech products and data formats must typically support. Now that the USCDI assists regulators in determining if a healthcare provider is engaging in information blocking or not. And all approved EHR systems in the United States must share data that maps to the USCDI v1 elements.
According to ONC, the guiding principles of USCDI are:
- Comprise a core set of data, both structured and unstructured, necessary to support patient care and provide patient access via health IT.
- Expand through predictable, open, collaborative processes considering expected benefits and industry-wide consequences.
- Create a uniform baseline of harmonized data pieces that may be broadly reused across use cases, including those unrelated to patient care or access.
Further, USCDI is the data point that anti-information blocking requirements require IT vendors to share commencing on April 5, 2021. Moreover, USCDI elements can also be used to build healthcare metrics and technology in the future. The USCDI, according to ONC, “is intended to grow over time as standards mature and users’ needs evolve.”
Conclusion
With this guide, we hope that you get a comprehensive understanding of EHR interoperability. In today’s growing digital health landscape, a seamless flow of information across healthcare systems, organizations, and entities is essential. Because data interchange will ultimately determine the success and efficiency of operations, care plans, etc. Interoperability in EHR is expanding, but still, there’s a long way to go. And the growing interoperability market is a clear indicator. Apart from that, with government initiatives and increased focus on patient-centric care models, the usage of EHRs is bound to go up. And so will the need for healthcare interoperability. Above all, it’s crucial to note that despite barriers to achieving interoperability, the standard frameworks, measuring methods, and ways to improve it are enough to boost it. And it wouldn’t be wrong to say that healthcare interoperability has a bright future in this digital care world.
References
- https://www.ibm.com/topics/interoperability-in-healthcare
- https://www.databridgemarketresearch.com/articles/healthcare-interoperability-the-new-growth-determining-force-driven
- https://tigerconnect.com/about/faqs/what-is-ehr-interoperability/
- https://www.himss.org/resources/determining-measures-success-interoperability
- https://blog.medisolv.com/articles/what-is-tefca
- https://www.healthit.gov/buzz-blog/health-it-policy/new-cms-rules-advancing-interoperability
- https://ehrintelligence.com/news/onc-releases-united-states-core-data-for-interoperability-version-3
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.