There are more than 100 potential COVID19 vaccines in different stages of development globally, and some are even undergoing clinical trials. The world is hoping for a successful outcome and waiting for things to get back to normal, but let’s face it – the post-Corona world will never be the same.
As all industries adjust to the new normal, the healthcare industry is also moving away from legacy systems and traditional healthcare processes. Adoption of advanced technological solutions helps in providing quality value-based care and improving patient outcomes. This article explores some trends that will define the patient management process by 2023.
Introduction to Patient Management
Patient management refers to all the interactions between a patient and the healthcare provider until the end of treatment including recording patient health information, explaining procedures and treatment plans, and recording physician’s post-visit notes, among other things. Patient management software systems combine data analytics and administrative tools that help in streamlining the various processes of care within a healthcare facility.
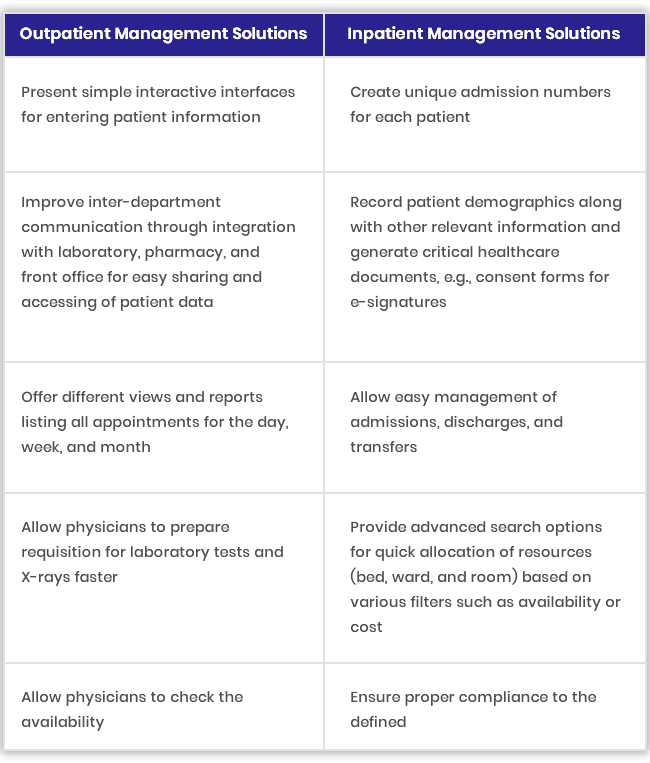
Outpatient and Inpatient Management Solutions
Patient management solutions automate several administrative tasks enabling providers to give enough time to each patient enhancing patient experiences and strengthening the patient-provider relationship. Intelligent patient management systems reduce the burden on healthcare professionals by allowing them to take notes, define parameters for each patient, and retrieve previous visit details quickly.
Healthcare organizations maintain patient data in two categories: inpatient management and outpatient management.
5 Solutions that will Define Patient Management by 2023
Healthcare organizations are adopting various emerging systems, tools, and services to provide value-based care to patients, enhance physician and patient satisfaction, and increase ROI.
Here are five solutions that seem poised to define patient management by 2023.
1. Point of Care Diagnostics
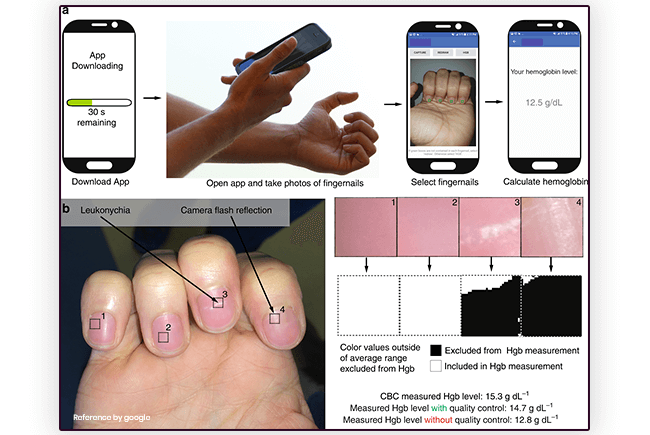
Point of care testing (POCT) differs from conventional diagnostic testing as testing is conducted at the patient’s bedside or remotely, and not in a laboratory.
Studies predict the global POCT market will reach $36.96 billion by 2021. The integration of POCT into established clinical practice facilitates quick medical decisions through early detection, monitoring, and treatment, leading to better patient outcomes. And integration of POCT with mobile healthcare (mH) solutions enhances patient engagement and lets patients take responsibility for their health.
- Acute stroke management: Portable and easy-to-use POCT devices help in the early diagnosis of strokes and allow grouping of stroke subtypes for effective management of chronically-ill patients.
- Cancer: Carbon nanotubes (CNT) are POCT devices that assist in the detection, drug transmission, imaging, physical ablation of metastasis, and therapy of cancer.
- Diabetes: Through cloud-based blood glucose monitoring POC devices, patients can share glucose readings with their healthcare providers from any location and receive timely intervention.
- HIV Testing: POCT methodologies make it easier for providers to reach rural populations and deliver faster results. Some POC tests allow physicians to screen and treat patients in a single visit by generating results in less than 70 minutes.
2. Remote Patient Monitoring
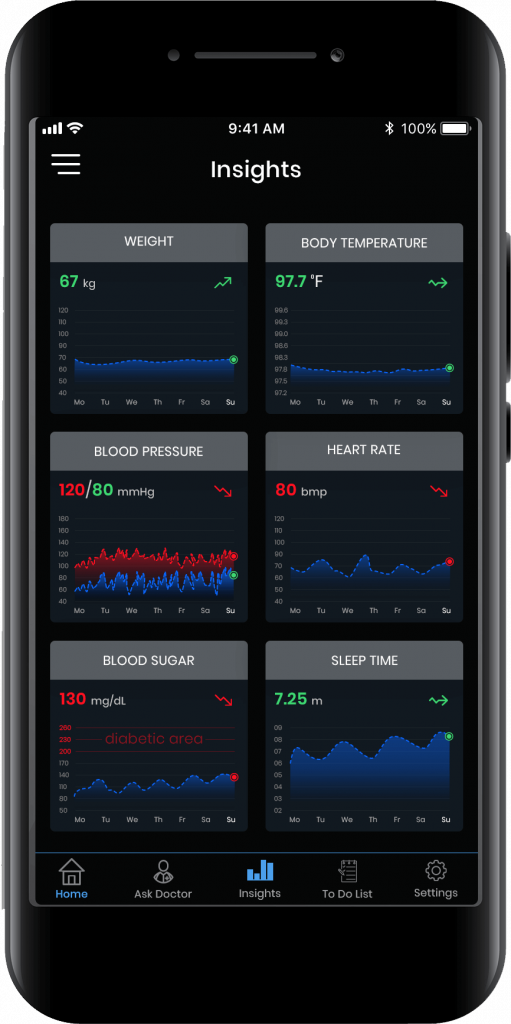
Care transparency is a critical element that will improve patient experiences and drive revenue as the healthcare industry shifts to a value-based care model.
Remote patient monitoring helps healthcare organizations provide better quality care services and enhance open communication between physicians and patients. The RPM system market is growing fast and is forecasted to reach $1789.4 million by 2025.
Remote patient monitoring solutions allow physicians to remotely monitor vital signs of patients, especially the elderly and chronically ill patients, in real-time.
RPM boosts the productivity of physicians as they can treat more patients, any time, anywhere. RPM products and devices also help in streamlining costs by reducing hospital readmission rates and making personalized care accessible to patients in remote areas.
Remote patient monitoring enhances patient engagement as patients and providers work together for effective management of their medical conditions.
- Prediction of Probability of Pneumonia – RPM systems determine the extent and location of the pneumonia infection in chest X-rays with complete accuracy. Healthcare providers can use this analysis to make critical decisions on the next steps.
- Post-surgery Monitoring of patients: Through RPM systems, physicians can remotely monitor a patient’s vital signs daily and intervene to avoid postoperative complications.
- Diagnosis of Deep Vein Thrombosis: Traditionally, an ultrasound helped to diagnose DVT. However, with the help of RPM devices, providers, and patients can monitor critical readings such as blood pressure, heart rate, SPO2, and device usage in real-time for early detection of DVT.
3. Health Analytics for Performance Management
Business intelligence techniques and data visualization tools in health analytics help healthcare providers to analyze the performance of various departments and processes within the organization and improve operational efficiency.

- Risk Scoring for Chronic Diseases – Risk scores generated using health analytics help in determining and managing high-risk individuals who will benefit from timely intervention.
- Reducing 30-day hospital readmissions rates – Intelligent health analytics monitor a patient’s risk factors and alert providers if there is a high likelihood of readmission within 30 days.
- Forestalling appointment no-shows – Providers can use health analytics to identify possible appointment no-shows and offer open slots to other patients.
- Predicting patient utilization patterns – Visualization tools and analytics strategies in health analytics systems anticipate peak utilization times. So emergency care clinics can rearrange scheduling procedures to maintain optimal staffing levels, minimize patient wait times, and improve patient satisfaction.
4. Social Determinants of Health (SDOH)
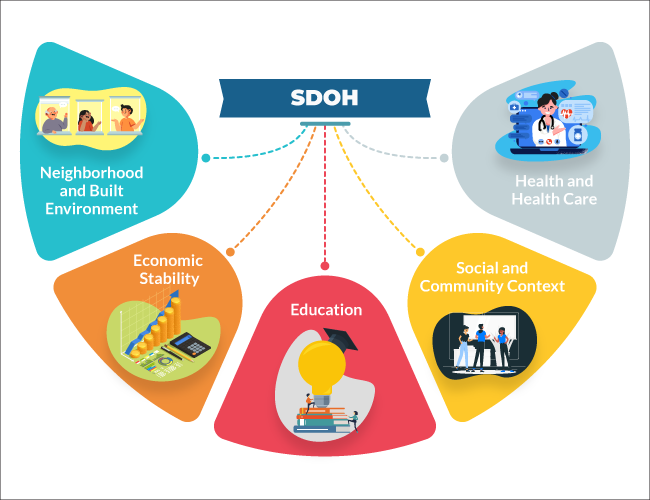
The social determinants of health (SDOH) include the social and economic conditions that affect a person’s health. Addressing these determinants will help healthcare organizations improve patient outcomes even after they leave the hospital.
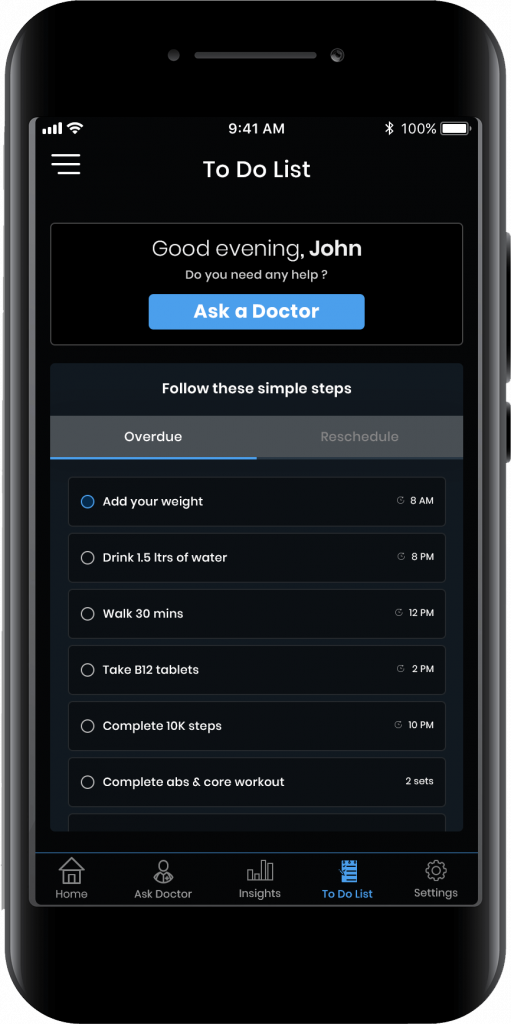
Remote patient monitoring and patient engagement through educational materials and health check-ins are some ways to enhance healthcare delivery.
Technology-driven solutions can improve patient outreach by addressing the following social determinants:
- Access – Advanced systems such as telehealth, e-prescription, and point-of-care test tools can help hospitals serve patients better and reduce operational costs in the long run.
- Telemedicine – Telemedicine systems can reduce physician burnout and help hospitals monitor patients remotely through simple interfaces.
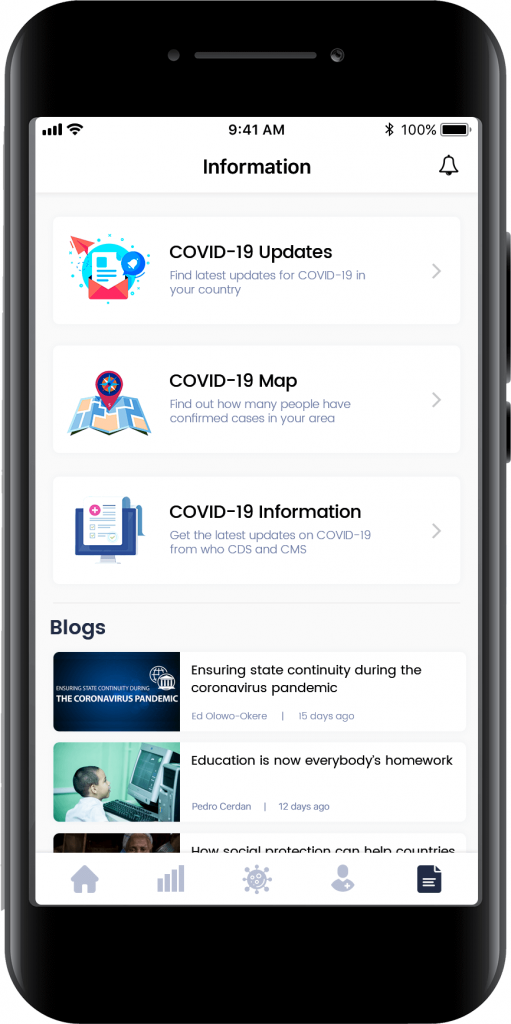
- Patient Education – Mobile healthcare apps can provide patients with detailed information about their health conditions and treatment plans. Patients can also track their progress, stick to the schedule, and receive daily personalized learning material.
- Community – Using technological platforms, hospitals can connect patients to organizations like shelters, food banks, schools, rehab centers, and grocery stores to improve health outcomes.
5. Care Collaboration
Proper coordination and communication between a patient’s multiple providers is vital for effective and quality care and maintaining consistency in the patient’s treatment plan.

Care collaboration also optimizes clinical procedures, facility management, and administrative tasks and helps in improving patient care services.
- Appointment scheduling efficiency – Collaborative scheduling solutions allow providers to view room availability of other providers and propose patient case discussions in open calendar slots.
- Real-time workflow visibility – Healthcare professionals can access patient data in the clinical workflow in real-time and prepare for appointments accordingly.
- Emergency Department patient flow – Healthcare workflow management solutions help providers to manage varying patient flows or a sudden increase in high-acuity patients daily without impacting ED efficiency.
- Streamline communication – Care collaboration can streamline communication between various providers for easy allocation of specialized resources backed by reliable data to improve patient outcomes.
Conclusion
Given the stiff competition in the healthcare industry and the innumerable challenges, healthcare providers must adopt intuitive and integrated healthcare management solutions. Some benefits offered by these systems are improved quality of services, enhanced patient engagement, reduced administrative errors, resulting in better patient management.
References:
https://www.pbmchealth.org/news-events/blog/difference-between-inpatient-and-outpatient-care
https://healthitanalytics.com/news/10-high-value-use-cases-for-predictive-analytics-in-healthcare
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.