Introduction:
Primary care is faced with several challenges that can adversely impact physicians and their care delivery, including integrated care or collaborative care. Some of the difficulties include: deciding the payment for primary care services and lowering the scope of practice for primary care physicians. Primary care practices invest tonnes of time following up patients, be it for appointments or payment reimbursement. This is where implementing telehealth in primary care comes into the picture and solves all dilemmas.
Telehealth services utilize electronic devices for supporting a wide range of remote healthcare services, such as remote patient monitoring and patient engagement. Telemedicine should be integrated into traditional ambulatory and hospital-based practices for accomplishing the full potential of population health management and practice management. Over the recent years, telehealth has transformed the industry by reducing costs and increasing electronic data exchange. Telehealth use has increased since 2020, and patients and providers understand its importance. It creates a safe atmosphere for patients to receive quality healthcare.
Benefits of integrating telehealth practices
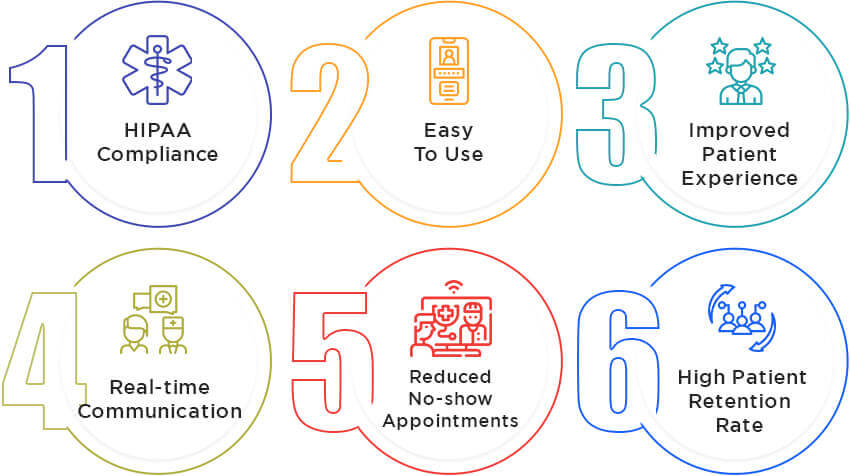
The amount of work in primary health services may spike burnouts among the administrative staff. Telehealth solutions can increase access to health informatics and improve healthcare analytics. Telemedicine software is safe and offers low risks. A telehealth software also saves time and greatly enhances health access to patients located anywhere. Telemedicine software companies allow doctors to focus more on the patients, resulting in better patient health outcomes.
Telemedicine software companies transitioned the traditional system of appointments and visits and implemented healthcare automation to manage tasks efficiently. Telemedicine solutions offer promising possibilities to primary care practices and enable effective care delivery to patients. Additionally, implementing telehealth in primary care helps advance new business models, enhances patient engagement, reduces patient costs, and increases ROI returns. Some of the key benefits of implementing telehealth in primary care are:
1. HIPAA-compliant Solution
Telehealth solutions safeguard from cybersecurity risks by utilizing digital health tools. Implementing telehealth in primary care offers EHR integrated platform that will protect your primary care services.
2. Easy to use
Telemedicine solutions are easy to use and can streamline the processes of healthcare practices. Telehealth software is convenient for patients to book appointments and communicate with healthcare providers. As a result, it brings patients back to the telehealth services, enhancing patient-provider engagement.
3. Improved patient experience
An EHR-integrated telehealth platform minimizes confusion and enhances patient experience. Telehealth systems are interoperable and provide patient portals, and Telehealth solutions enhance health access to improve the patient experience.
4. Real-time Communication
One of the main advantages of telehealth solutions is seamless real-time communication. This may change based on the telehealth alternatives you want to offer in your clinic. But the virtual connection makes it much simpler to maintain communication between provider and patient. Offering your patients a way to stay in touch with you will make connecting easy when necessary and foster your relationship.
5. Reduced No-show appointments
There are no more justifications for no-show clients, thanks to telehealth solutions. It enables you and your patients to communicate more easily, and there is no need to even travel to the clinic. Telehealth allows more customers to meet with you because it is simple, convenient, and frequently results in shorter session times. Moreover, implementing telehealth in primary care clinics will increase their savings by reducing no-show appointments.
6. High Patient Retention Rate
Patient engagement has been demonstrated to rise with telehealth. When your clients stay on schedule, they experience faster-than-ever outcomes. All of this results in higher satisfaction and improved retention. By doing this, you may retain your current clients coming back to you for appointments week after week.
Top Challenges Practices Face in Implementing Telehealth
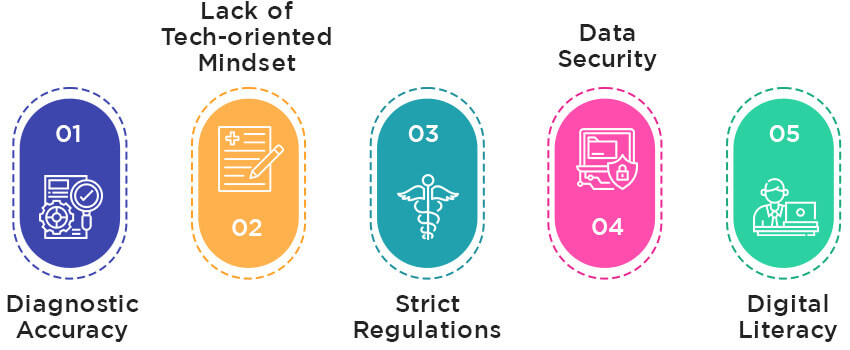
It’s undeniable that the telehealth market is rising rapidly. But challenges in its implementation still exist. Here are some barriers practices face when implementing telehealth
1. Diagnostic Accuracy
One of the primary issues with telemedicine is using digital tools for patient examinations. Misdiagnoses can also occur in in-person healthcare, but employing remote care has a far larger risk. Misdiagnoses can be harmful to people and medical practitioners. After all, inaccurate diagnoses can result in inappropriate prescriptions and potentially hazardous treatments. They significantly raise the cost of care. Implementing telehealth in primary care is hindered by these problems for patients and doctors who desire to reduce the risk of medical mistakes and malpractice.
2. Lack of Tech-oriented Mindset
The lack of a tech-oriented mindset is one of the biggest obstacles to telemedicine solutions in rural areas. In those regions, 87% of doctors still conduct patient transactions using paper and manual methods. Also, there are a lot of smaller medical offices with little incomes (up to $150,000 annually) and traditional doctors who do not wish to use modern technologies.
3. Strict Regulations
One of the main issues with telemedicine is the stringent regulations. Telehealth platforms must comply with HIPAA regulations like any other healthcare provider’s solutions. A healthcare provider may be penalized if they are not. Penalties for HIPAA infractions can range from $100 to $50,000 per offense. The HHS Department has lowered the HIPAA criteria for telemedicine software during the pandemic to help providers reach more patients. It specifically stated a restricted exception from HIPAA penalties for using technologies that would not fully abide by HIPAA regulations during a public health emergency. But these HIPAA limitations are only temporary. Long-term obstacles to providers adopting telemedicine solutions include strict regulations and steep fines.
4. Data Security
Medical providers hold a lot of sensitive data, which makes the industry a soft target for data breaches. The HIPAA 2019 Healthcare Data Breach Report states that over 41.2 thousand stolen medical records affected the healthcare sector immensely. This figure is likely substantially higher today, given that phishing scams and ransomware spiked 350% during the pandemic. As telehealth solutions give hackers new entry points, it poses an even larger danger of data-related breaches. Moreover, this implies that healthcare providers must spend more money to provide technologies with strong security, interoperability, and encryption features. So, the biggest barriers to the implementation of telehealth in primary care are rising costs and the danger of data leakage.
5. Digital Literacy
About 7% of Americans don’t have internet access, while 25% of people 65 and older never use it, as per a 2021 Pew Research Center survey. In other words, nearly tens of millions of individuals are cut off from telehealth services because they cannot participate in video conferences with medical professionals. Another serious barrier to implementing telehealth in primary care is low digital literacy. For instance, elders with access to technology may sometimes be technically competent. Some people need help to set up an account, make a phone call, or comprehend how a smartphone’s frontal camera functions.
Top 5 strategies for implementing telehealth
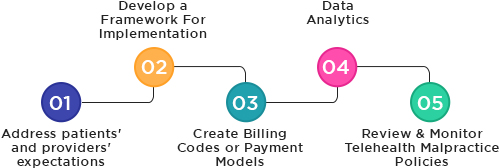
1. Address patient’s and provider’s expectations
Telehealth software companies need to provide better care management from home, which can also apply to chronic care and management of health conditions among the elderly. For instance, patients must reach out to neurologists through telehealth systems seeking medical help or guidance. Similarly, a telehealth solution also should serve as beneficial for dealing with mental health issues. Patients in need of counselling or therapy no longer need to travel for in-person visits and receive immediate attention virtually. Utilize telemedicine software platforms to give the flexibility of allows doctors to conduct a health examination remotely. Make sure the telehealth solutions are interoperable from any device.
2. Develop a framework for implementation
While implementing telehealth in primary care, it is important to have a clear structure. Set clear goals for your advanced telemedicine and create a realistic plan for achieving them. Have a clear picture of how you would like the telemedicine software for providers to be implemented in your primary care practice. Plan the integration of advanced telehealth solutions, keeping in mind your staff. Make your team familiar with the integrated telehealth solutions and provide them with the support needed for the transition. It is also necessary to acquire feedback from staff and patients to understand their experience with your telehealth software systems.
3. Create billing codes or payment models
One of the major concerns of using a telehealth app is to get the right CPT codes for filing medical billing claims. Billing through a telemedicine app or mHealth app can seem confusing, but the codes used for the process are the simplest ingredients for successfully implementing telehealth in primary care. Like with any insurance claim, telehealth apps could face payment issues. That is why it is vital to establish billing codes or payment models to manage payments. You need to make sure your medical claim management and medical billing with a telemedicine platform point in the right direction.
4. Data analytics
Telemedicine apps are an example of merging technology with healthcare services. One of the major aspects that have transformed healthcare analytics. A telemedicine app for doctors utilized tools and approaches for predictive analysis that helps physicians to keep tabs on patients’ health conditions. Telemedicine software development involves deep data analytics that can analyse large data sets of patients using virtual care and predict their health. Big data forms an integral part of a telehealth app for patients, which is why you need to ensure your telehealth mobile app can perform real-time data analytics. Telemedicine should be able to manage data sets accurately and at the same time ensure HIPAA compliance and security.
5. Review and monitor telehealth malpractice policies
Implementing telehealth in primary care comes with exposure to malpractice risk in direct-to-consumer telemedicine. Cloud-based telehealth services can regulate patient identity verification, suboptimal diagnosis and treatment, and inadequate medical history. Implementing telehealth in primary care can be subjected to malpractice litigation. The malpractice risk of DTC in telehealth solutions needs to be looked into. You must monitor the telehealth practices to identify gaps or malpractices.
Conclusion
Telemedicine mobile apps for primary care can change the way patients perceive healthcare and experience health services. OSP can develop telemedicine applications for healthcare to help you increase your ROI returns and improve the patient experience. We can help you with telehealth implementation through our strategic planning and experienced software developers. Our custom software solutions can simplify the telehealth implementation strategy for medical records management.
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.