‘Tell me about your experience and educational background,’ sounds familiar? Chances are you must have faced this classic job interview question at least once in your lifetime. A person or business with good credentials finds favor in every profession and industry. This article deals with healthcare credentialing, the advantages of automated provider credentialing, and 10 features you should look for in healthcare credentialing solutions.
Introduction to Credentialing Software
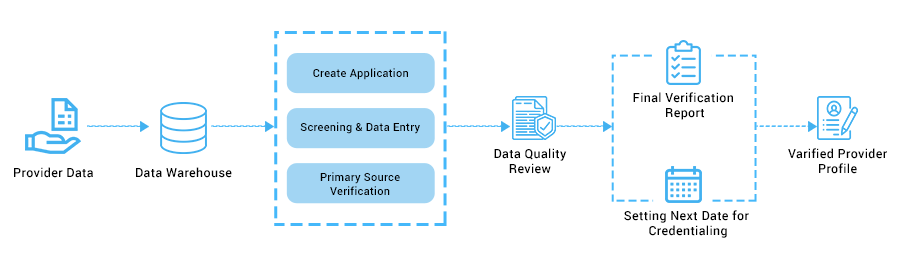
‘Credentialing’ can be loosely defined as a process used to assess the educational background, training, and practice history of a medical provider. Provider credentialing has existed for centuries, but it was only around 1990 that national organizations gave credentialing a formal structure. These organizations defined the criteria for credentialing physicians, physician assistants, and nurse practitioners. One of these criteria is the confirmation of the board certification, qualifications, malpractice claims, etc. from the primary source of the credential.
Credentialing software helps healthcare providers save time, money, and minimize errors as work previously done using stacks of paper forms, spreadsheets, and emails are automated.
Do healthcare providers really need credentialing software?

- Healthcare credentialing software allows healthcare organizations and insurance companies to store and manage the records of healthcare providers. It also ensures they have the essential licenses and certificates to work as a medical practitioner. From a patient’s perspective, the credentialing process provides them an assurance that they are in qualified and competent hands.
- A healthcare provider who is a part of the credentialing software is assured that all other medical professionals are following the same standards as you. Also, it tells you that a prospective employer believes in providing quality and reliable healthcare to its patients.
Manual Credentialing Vs. Automated Credentialing
If you are still unsure whether you should opt for an automated credentialing solution or stick to manual credentialing, this table presents some of the benefits of automated credentialing.

Mistakes in Credentialing Process
Credentialing process in healthcare is not a breeze. One mistake and the physician’s whole career could be in jeopardy. And the consequences could be catastrophic. From financial losses to legal complications, credentialing mistakes can make physicians and healthcare facilities suffer. What can those mistakes be? Below are a couple of mistakes that can happen in the credentialing process. Take a look-
1. Mistakes in Planning
It’s a known fact that credentialing process takes time. Loads of document collection and verification take a couple of months to complete. Sometimes it can take more time. The biggest mistake the healthcare facility or staff can make is to fail to plan for this delay in the process. And both HCP and facility suffer.
The healthcare professionals’ time is at stake, as they can only render care services if they are credentialed. Moreover, the healthcare facility can only get reimbursed if the caregiver is credentialed. It’s a financial loss for the healthcare company. So, proper planning, keeping in mind the potential time frame, is important to avoid losses.
2. Errors in Data Entry
Making human errors in filling out the credentialing application is quite a common mistake. There are different types of errors that can cause the delay or denial of the application. Well, typo errors are quite common mistakes that happen while entering data. Missing words or interchanged information leads to clarity. It’s best to do a quick revision after entering the data for errors.
Another mistake in the credentialing process is missing out on relevant data or completely omitting a required document. These mistakes stand out and create havoc in the process. Apart from these two, poor handling of documents also creates ambiguity and confuses the application process. It also leads to resubmissions.
3. Inaccuracies in the Application Process
Not only do mistakes happen in data entry, but inaccuracies in the application process can also cause delays and rejection of the credentialing application. Aspects that can potentially go wrong are-
Delays due to clinical staff: Understandably, clinical staff are super busy. Often they need to respond to queries and doubts arising in the application process.
Incomplete application: Leaving important places blank or not attaching relevant documents often falls under the incomplete application category. It leads to confusion, and sometimes the application also gets rejected.
Failure to track the application status: Negligence might only sometimes happen from your side but also from other parties involved in the credentialing process. Sometimes insurance providers might cause delays in processing the credentialing application, so clinical staff needs to keep track of the application at every stage. Failure to do so is also a mistake for the clinical staff.
Authorization mistakes: Credentialing applications require signatures and attestations of the specific party. Any mistakes in this can lead to the rejection of the application.
4. Mistakes in Enrolment Process
As the enrolment process is about billing and payments, any mistakes directly impact the revenue cycle. Some common incidents that are marked as mistakes are-
Need to meet insurance providers’ criteria: Insurance companies also set credentialing regulations, including protocols, timelines, and more. Meeting these criteria can ensure the credentialing process is successful.
Having no contacts with Insurance companies: To get credentialing done for practice or physician, it’s crucial to know the insurance companies in that area.
5. Compliance Errors
There are different state requirements for credentialing, and staff needs to be careful about these compliance requirements. Failing to be compliant is a major issue of credentialing in healthcare. Some reasons are-
Lack of complete knowledge: If staff responsible for credentialing process is ignorant about the regulations and other requirements, it can mess up the whole process.
Lack of knowledge of the specialty: As every specialty has specifics, it’s essential to have full knowledge about the specialty being practiced. It’s crucial to prove the competency for the specialty through required documents, which ensures smooth credentialing.
Non-compliant with specific regulations: Since every insurance company has its own set of regulations, it’s the responsibility of the practice or physician to ensure compliance with those specific regulations.
Lack of legal implications: As mentioned before, credentialing mistakes can lead to legal consequences. Another issue is that many staff need to be made aware of the legal implications of credentialing, which they must have.
6. Lack of Digital Support
As the credentialing process is quite complex, doing it manually is an uphill task. Opting for digital support like credentialing software can make the process faster and less complicated. The staff handling credentialing process can only sometimes be updated with state and private companies’ regulations if done manually.
Moreover, staff might miss deadlines, considering they have other administrative chores. Plus, they can’t track the application as well. And these can result in severe consequences, as you can imagine. Getting credentials is a task; renewing them before it expires is another job. And as mentioned, clinical staff have a busy schedule, and forgetting the renewal dates is quite possible. In all these expected complexities of the credentialing process, deploying software can make staff’s job a lot easier.
Challenges in Healthcare Credentialing Software
Implementing healthcare credentialing software can be challenging owing to some specific roadblocks. As medical credentialing is a complex process, deploying credentialing software can make the process a breeze. However, facilities, physicians, and developers still have some obstacles in the implementation process-
1. Lack of Privacy and Security
Ensuring the practice’s background is essential for credentialing software. Not just of the health practice but also the independent applicant. Background checks can reveal much about the practice’s malpractice, board actions, or other reports to NPD. And securing and keeping this information private is important for credentialing and insurance organizations.
2. Ensuring Compliance with State Regulations
Implementing credentialing software can be affected due to constantly changing state regulations. As every state updates its credentialing regulations, keeping tabs on this is important. And ensure compliance when deploying the software.
3. Inability to Access Updated Information
In medical staff credentialing software, up-to-date information is a must. Without having access to up-to-date information can make the implementation process more complex or delay it. The healthcare practice must provide developers with updated information to ensure smooth implementation.
4. Inability to Switch Platforms
Credentialing in healthcare platforms can require integrations with more needs. Integrations with other platforms can easily cater to practitioners’ varied needs. However, integration or migration won’t only be possible if the platform has content compliant with regulations. And this can affect the healthcare credentialing software in the long run.
5. Unable to Meet Deadlines
Meeting deadlines is a must in the medical credentialing process. The inability to meet deadlines can cost the healthcare practice a lot. Deploying the healthcare credentialing software with a reminder feature can only resolve this problem and ensure seamless credentialing.
How to Choose the Right Credentialing Software for Your Organization
There are several credentialing software systems available in the market currently that include the basic features like data storage and online verification. However, if you wish to make your organizations’ credentialing process more effective and proficient, look for credentialing software that includes the 10 features listed below.
1. Centralized Credentialing
Centralized credentialing is a process whereby two or more healthcare facilities reduce costs by dividing the total cost of credentialing providers. The good news for providers is they only have to go through the lengthy credentialing process once, and also increases the goodwill between providers and administrators. Other advantages of centralized credentialing include enhanced credentialing efficiency, easier facilitation of delegation with payers, and improved data integrity, all of which boosts revenue cycle management.
2. Cloud-based System (Total Portability)
Portability will not be an issue if you opt for a credentialing software solution that saves the data on the cloud. This will ensure that all the users – your organization’s employees and the providers – can use the credentialing system on any digital device with complete security.
3. CAQH Integration
The Council for Affordable Quality Healthcare (CAQH) is a non-profit association of health insurers that collects and maintains a database of provider credentialing data. Customized credentialing system integrated with provider credentialing information from CAQH will make it easier to share provider data accurately and efficiently with multiple health plans in one go.
4. Workflow Automation
The credentialing process involves the collection of data from the healthcare providers, development of the credentialing strategy, verification of the given credentials and licenses, management of provider profiles, and getting in touch with payers. Credentialing software tailor-made with real-time, intuitive dashboards, and automated workflows for online verification, attestation aging, expiration management, credentialing metrics, and onboarding options will considerably enhance productivity.
5. Document Expiration Management (Alerts and Reminders)
Healthcare facilities using manual credentialing face challenges in regularly updating providers’ data and credentials. However, credentialing software built according to your requirements can help to keep track of the provider’s profile as well as documents and certificates nearing expiration and changes in performance metrics. You can also configure expiration reminders and alerts to send automatic notifications and email reminders to the staff responsible for these tasks.
6. CME Tracking (continuing medical education)
Learning never ends for physicians and other health professionals who are committed to improving patient care. However, tracking continuing medical education (CME) activities can get very tricky. When choosing credentialing software, look for a system that offers professionals a streamlined process to earn, track and view reports on CME certifications, CME credits, and certification points.
7. Electronic Forms and e-Signatures

In a medical facility, every second count, and sometimes, waiting for certain medical consent forms or signatures can prove to be costly. Credentialing software solutions with comprehensive and robust systems that allow for the use of electronic forms and e-signatures can greatly benefit healthcare professionals.
8. Peer Review Process Automation
Medical peer review is a measure used to improve the quality and safety of patient care. In this process, healthcare professionals evaluate the performance of current and former colleagues to ascertain the accuracy, relevance, and significance of their work. If the credentialing software system acquires, combines, and saves feedback for the provider obtained from peers, this will help the peer review process run smoothly.
9. Secure Database Management

We all know how important data is, and yet, if not managed efficiently, the same data can pose a big problem. In manual credentialing, healthcare facilities struggle with handling providers’ data. A personalized credentialing software system with comprehensive end-to-end functionality takes care of all aspects of data management such as data storage, data segmentation, and data security.
10. Customized Reporting
With automated credentialing, you no longer need to rack your brains, creating different reports to figure out how each parameter impacts the workflow process. Intuitive, comprehensive, and customized credentialing reports available in credentialing software systems use an ad-hoc report writer to recover insightful data and customize reports with top-quality features including institutional summary, days in enrollment, facility summary, provider summary, etc.
Conclusion
Every year, healthcare facilities spend a considerable amount of time and money on provider credentialing. A healthcare facility’s complete revenue cycle depends on proper medical credentialing. Any errors in insurance credentialing cost you valuable time and money in addition to increased legal liability, and coverage and referral issues. Invest in a customized credentialing software solution to streamline this expensive, time-consuming, and complex process and boost your organization’s income and efficacy.
OSP can program a custom-made healthcare credentialing solution to help you credential smarter and faster. We have experience in building top-notch credentialing solutions that can eliminate administrative paperwork and replacing it with a simplified credentialing solution. Learn how we helped a mental health provider in Texas to solve their credentialing challenges here.
Want to See it in Action?
OSP is a trusted software development company that delivers bespoke solutions as per your business needs. Connect with us to hire the best talents in the industry to build enterprise-grade software.

How can we help?
Fill out the short form below or call us at (888) 846-5382
Looking for software solutions to build your product?
Let's discuss your software solutions for your product in our free development acceleration call!
Get In Touch arrow_forwardDiscuss Your Project Handover with a team of expert Book a free consultation arrow_forward
About Author

Written by Riken Shah linkedin
Riken's work motto is to help healthcare providers use technological advancements to make healthcare easily accessible to all stakeholders, from providers to patients. Under his leadership and guidance, OSP Labs has successfully developed over 600 customized software solutions for 200+ healthcare clients across continents.