Blogs
Enhancing the Abilities of Healthcare SectorServices
Solutions
Services
Solutions
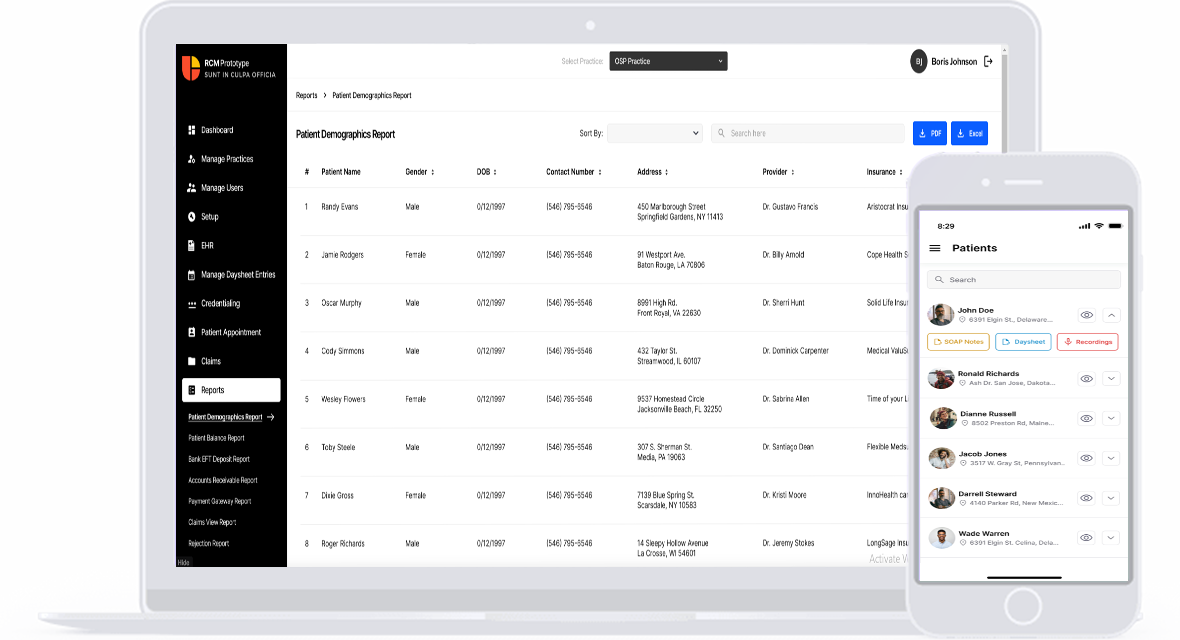
OSP engineered a cutting-edge revenue cycle management solution with multiple core capabilities and additional features. Our RCM platform is built with a wide spectrum of features that will cater to the different billing and revenue cycle needs of your practice. Besides, this RCM software also has additional features that will help providers boost care delivery and patient experience. With core features and additional capabilities, our RCM solution is well-equipped to resolve all billing and practice management issues. Additionally, our practice management RCM software even offers third-party integrations to streamline workflows and processes. This RCM system is specifically designed and developed by OSP to resolve various challenges faced by healthcare providers today.
Increased Net Revenue
Reduced Billing Costs
Years of Experience
Our cloud-based RCM solutions effectively manages medical records. This streamlined RCM solutions store patients’ demographics, billing, insurance eligibility details, emergency contacts, ledger, and other forms. Integrated with EHR/EMR systems, our RCM services provide patient details. This feature enables providers to access patient data easily at one centralized location. Also, integration with electronic health records reduces the burden of manual entry. With this feature, our RCM services enable providers to focus more on delivering quality care. Besides, this feature also reduces the chances of human errors and inaccuracies in medical records.
Learn more
OSP’s RCM software products featuring provider data management streamline all records related to healthcare practitioners. Our revenue optimization solutions offer providers personal and professional information. Besides, the revenue cycle management software effectively manages malpractices incurred by doctors/practitioners. This feature ensures providers can directly view, assess, and manage their data. Our RCM technology platform with provider data management capability also manage different documents of providers efficiently. With documents, the platform even manages certificates and licenses of providers. Overall, provider data management helps insurance companies and practices keep track of the eligibility of providers.
Learn more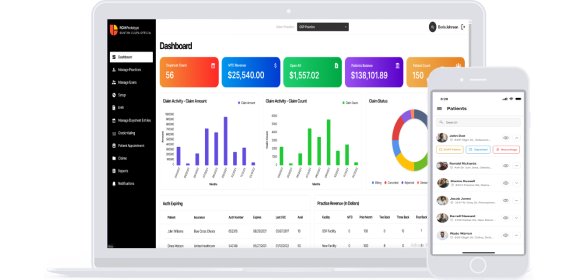
As we developed this practice management RCM software, we ensured to include master data management capability. This medical billing and RCM platform has the ability to manage CPT codes, which includes the comprehensive fee schedule. With this ability, our platform leaves no room for errors and inaccuracies. Further, this healthcare revenue cycle suite also manages aspects such as ICD, place of service, insurance, taxonomy, facility and submitter. This ability enables providers to submit accurate bills with proper coding and other information. That means, with this capability, our RCM software solution can minimize denials and delays, and improve revenue generation.
Learn more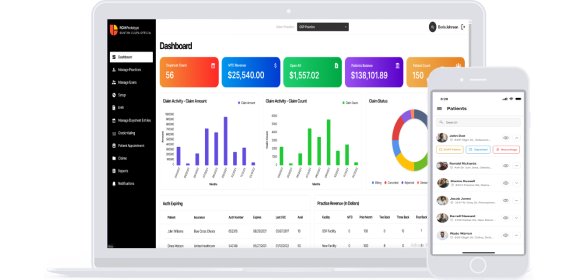
We designed and developed the healthcare revenue management platform with the medical day sheet management capability. This feature ensures accurate billing, revenue optimization and even compliance. With this feature, providers get day to day summary of patients’ encounters or care episodes. This will help practitioners track and document all billable services. Further, the feature also helps providers prevent missed charges, reduce coding errors, and minimize claim denials. Above all, this feature improves the operational efficiency of practice, boosts revenue collection, and even contributes to the financial health of practices.
Learn more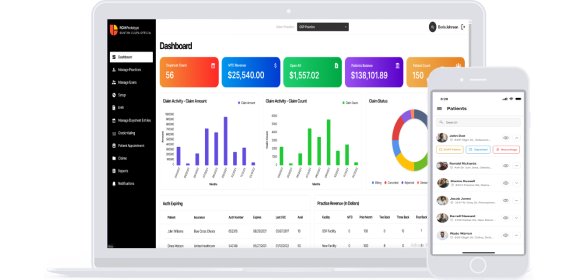
Our revenue cycle data management solutions also feature claims submission and processing capability. This feature is quite critical to providers, as it enables them to submit claims seamlessly and accurately. Besides, this feature in our hospital RCM technology submits claims in two key formats- Electronic 837 and HC1500 paper claims. These paper claims’ formats ensure compatibility with traditional workflows. Our RCM for healthcare providers also caters to their different needs owing to this duality. Healthcare providers can easily submit accurate claims using this feature. Overall, our RCM billing and claims software with this feature ensures timely claim submission, which will optimize revenue and maintain financial stability.
Learn more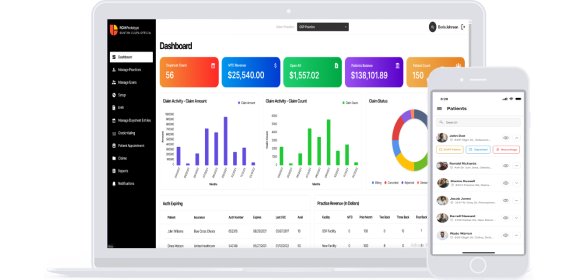
OSP’s advanced RCM software comes with a powerful claims rule engine. This feature is designed and incorporated into our platform to optimize claims processing and reduce denial rates. This claims rule engine excels in three crucial aspects, which include handling supervisor logic, modifier logic, and substitute carrier code logic. Dealing with these components, the engine enables the software to process claims accurately and promptly. Further, it also reduces errors and accelerates the reimbursement process.
Learn more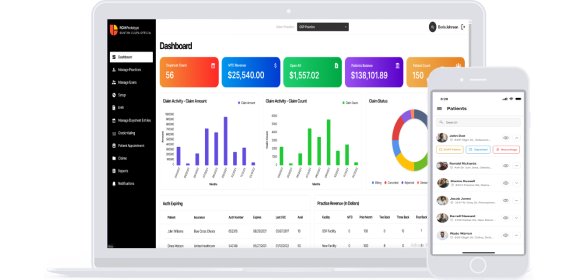
Insurance eligibility verification is a critical feature of our hospital revenue cycle software. This game–changing feature streamlines the revenue cycle by enabling providers to confirm the eligibility of patients’ insurance coverage and other benefits. This automated insurance eligibility verification enables providers to accurately estimate patients’ responsibility and reduce claim denials due to eligibility issues. Inclusion of this verification capability in our RCM platform not only improves revenue predictability but also patient experience. It helps patients to stay well-informed about their healthcare financial responsibility.
Learn more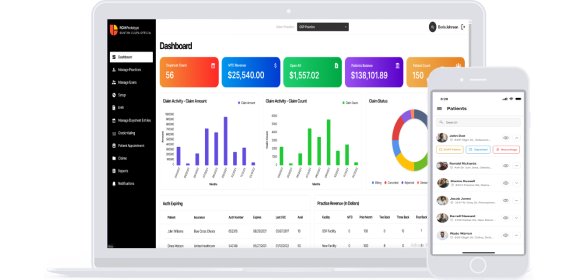
Another pivotal feature of our RCM solutions is A/R management. This feature is crucial in optimizing the revenue cycle for practitioners. We designed our RCM automation platform with this feature to empower providers in managing outstanding claims and patient balances. Further, this feature also offers tools to track, analyze and follow-up on unpaid claims and dues. As a result, it reduces A/R aging or cycle and speeds up the cash flow. Besides, this feature also enables providers to identify and manage revenue leakage, streamline billing process and improve financial performance.
Learn more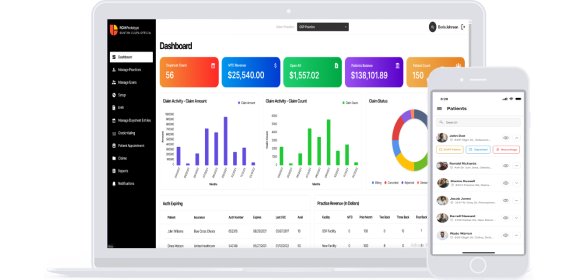
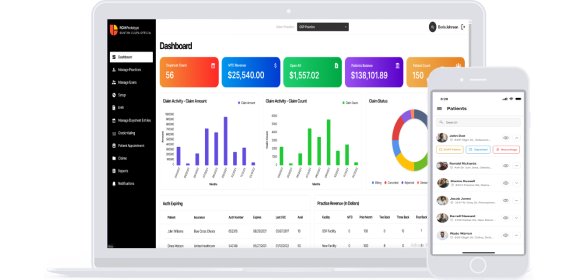
Our RCM solutions revolutionize the revenue cycle for providers through its analytics feature. This RCM analytics for revenue growth offers providers data-driven insights and performance metrics. And these metrics enable providers to make informed decisions, optimize processes and even improve revenue capture. Further, our RCM analytics tools also enable real-time tracking of KPIs and identify bottlenecks in the revenue cycle. It also helps providers to adapt to changing reimbursement models. This feature, in short, boosts efficiency, reduces costs, minimizes claim denials and helps providers achieve financial stability.
Learn more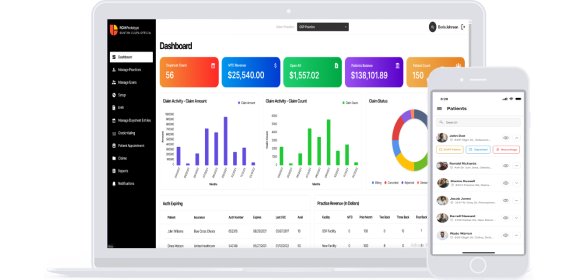
Our RCM application also includes Prior Authorization as one of the core features. This feature streamlines the complex and time–consuming process of obtaining pre-approvals for medical procedures and services. Besides, with automation and optimization of prior authorization processes, our RCM software solution enables providers to reduce administrative burdens. The platform with this feature even improves care coordination and ensures timely intervention for essential treatments. Above all, this feature incorporated in our RCM system reduces claim denials and increases revenue capture.
Learn more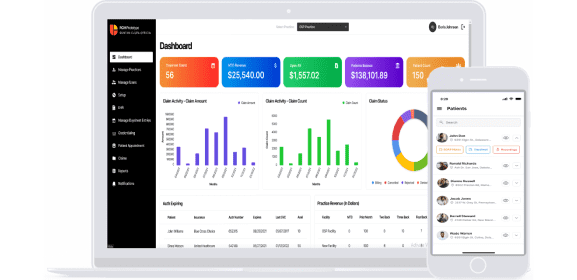
Integration with clinical notes assists practitioners in maintaining comprehensive patient records. It is an important feature for accurate coding and billing. This ensures claims are aligned with comprehensive patient data. These notes include critical information related to a patient's medical history, symptoms, diagnosis, treatment, and other relevant data. These notes also include insurance claims, reducing denials, ensuring compliance, and offering legal protection. Additionally, they enhance patient care through comprehensive patient history and progress tracking.
Learn more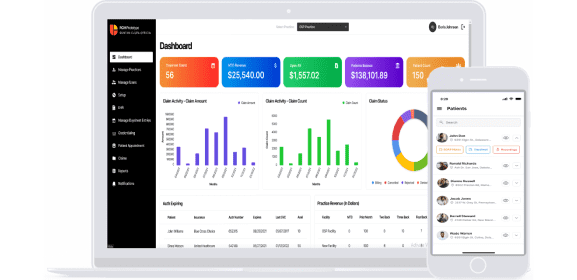
Telehealth integration with our RCM software benefits practitioners and patients by enabling virtual appointments. It facilitates billing through RCM software and patients can access it easily. Integrated with EHR systems, it offers analytics and reporting to optimize financial performance in virtual care, enhancing the patient experience. This feature promotes healthcare flexibility, facilitating consultations and billing processes that benefit both practitioners and patients.
Learn more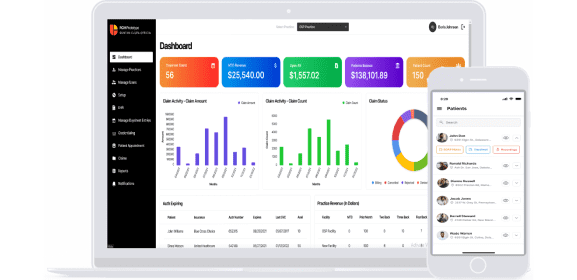
The credentialing feature, if added to our RCM software, will streamline the management of healthcare provider qualifications. It ensures that practitioners meet the requirements and standards of regulatory bodies and insurance providers. Besides, this process enhances compliance, reduces administrative burdens, and facilitates seamless participation in healthcare networks, ultimately supporting accurate billing and efficient revenue cycle management.
Learn more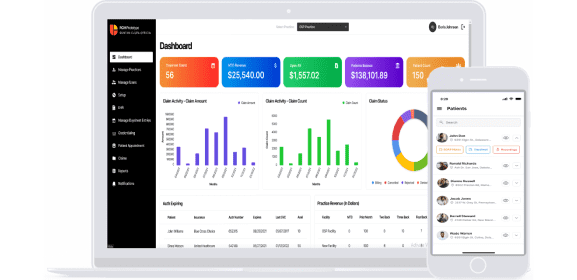
Chatbots integrated with our RCM software boost patient engagement by providing quick responses to common queries. It assists in guiding patients to the right resources and information, reducing the workload on administrative staff. Besides, this feature fosters effective communication, helps in addressing patient inquiries, and contributes to a smoother billing process.
Learn more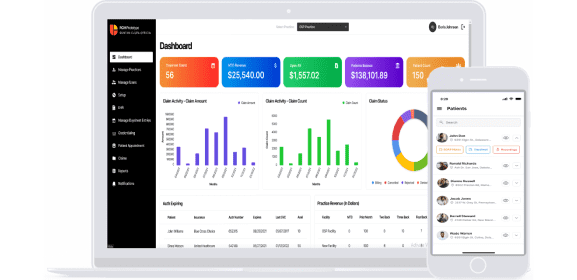
The postal feature integrated with our RCM software refers to the capability of mailing patient statements, reminders, or bills as part of the billing and financial communication process. It ensures that patients receive physical copies of their billing information through traditional postal services. These features serve as an additional avenue for providing billing details, enhancing patient awareness of their financial responsibilities, and supporting the revenue collection process.
Learn more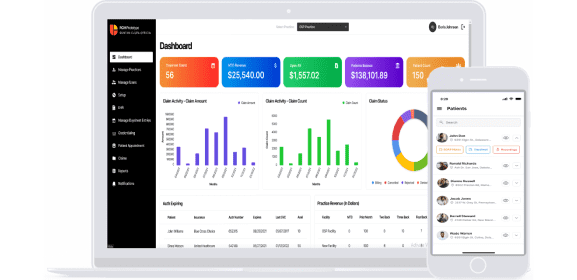
E-prescription features enable healthcare practitioners to transmit prescriptions to pharmacies electronically. This feature streamlines the prescription process, improving efficiency and patient safety. It eliminates the need for paper prescriptions, reducing errors and ensuring that patients receive the correct medications quickly. Besides, it supports accurate billing by seamlessly integrating prescription information into the revenue cycle.
Learn more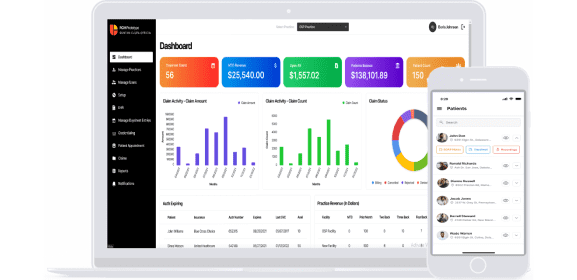
Our RCM software integrated with a digital wallet feature, simplifies the payment process. It streamlines the payment process by securely storing payment information, enabling patients to pay their medical bills online. This feature enhances patient experience by providing an efficient and user-friendly method for settling financial obligations related to healthcare services.
Learn more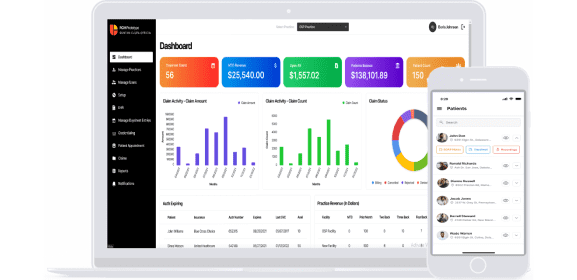
Virtual assistance integrated with our RCM solution serves as a digital tool that guides patients through the billing process and answers their inquiries. It provides real-time assistance, helping patients understand and navigate billing procedures better. This feature enhances patient engagement and reduces the workload on administrative staff, ensuring a smoother billing experience.
Learn more
Integrated with our RCM software to ensure the accurate billing of appointments. It helps practitioners manage and schedule patient appointments efficiently. By coordinating appointments with the billing process, this feature ensures that healthcare services are billed correctly and aligned with the revenue cycle, facilitating smoother patient care and financial operations.
Learn more
Integrated with our RCM software, Payment Gateway Integration facilitates online payments from patients. It seamlessly connects the software to payment gateways, allowing patients to make online payments for medical bills. This feature enhances the payment process, providing patients with a convenient and secure way to settle their financial obligations while streamlining the revenue collection process for practitioners.
Learn more
With patient statement solution integration, practitioners can streamline billing by generating and sending statements to the patients. This ensures that patients receive clear and accurate statements of their healthcare expenses. Besides, this feature helps patients understand their financial responsibility by providing transparency in financial communication. It also reduces billing inquiries and supports efficient revenue cycle management for practitioners.
Learn more
Internal communication integration with our RCM software facilitates secure messaging and communication among healthcare staff within an organization. It enhances collaboration and coordination among staff, enabling efficient and confidential communication regarding billing, coding, and other revenue-related matters. Besides, this feature supports streamlined internal processes and contributes to effective revenue cycle management.
Learn moreOSP’s RCM software accelerates the collection process through streamlined claims submission and proper reimbursement tracking. This results in quicker payments, which ultimately leads to steady cash flow for providers.
By leveraging RCM automation, our platform reduces tedious and time-consuming tasks. With the reduced burden on billing staff, the software improves overall productivity and allows staff to focus more on value-added activities.
Our RCM solutions help identify and resolve billing errors and discrepancies quite early in the revenue cycle. As the software ensures accurate coding and proper documentation, there are reduced claim denials and accumulation of bad debt.
Our integrated RCM software accelerates the complete A/R process, from claims submission to payment collection. By shortening the A/R cycle, the platform reduces the waiting time for reimbursement for providers.
Our RCM technology platform provides meaningful insights through data analytics. Leveraging these financial data, healthcare providers can make informed decisions related to revenue optimization, cost control and so on.
Our RCM software makes sure patients receive proper and accurate billing statements. Also, the software ensures that patients have convenient payment options. This transparency can lead to patient satisfaction and increased loyalty.
Our RCM software streamlines claims processing and submission by automating tasks like identifying covered services, generating medical claims, and submitting them to insurers. It also helps reduce claim denials and accelerates payment collection from patients. Our software features include automatic account edits, EMR integration, online claim submission, and automated billing. It saves time by automating patient appointment reminders, balance notifications, and communication with insurers for claim denials.
Our RCM technology offers integration with payment gateway, audio/video service, email service, SMS service, clearing house service, and notes services, with existing systems.
Our product provides insights into security features such as encryption for safeguarding electronic data transmission, secure networks to thwart unauthorized access, adherence to HIPAA regulations to uphold patient data privacy, data backup, and recovery capabilities to mitigate potential data loss due to system failures or cyberattacks, access controls for limiting data access to authorized personnel, and the presence of audit trails to track data access and user activity, ensuring patient data confidentiality and integrity.
Our software offers robust data analytics capabilities, including built-in analytics that offer a comprehensive view of RCM performance, enabling productivity and profitability enhancements. the revenue cycle management software effectively manages malpractices incurred by doctors/practitioners. This feature ensures providers can directly view, assess, and manage their data.
To ensure compliance with healthcare regulations and billing standards, our RCM solution enables accurate coding and documentation to mitigate audit risks and penalties. Adherence to HIPAA regulations safeguards patient data privacy. Compliance protocols within the software ensure conformity with healthcare regulations, payer requirements, and coding guidelines. Robust data security measures, including encryption and secure networks, protect electronic health information transmission. Our software helps providers stay informed about evolving government regulations and mandates affecting healthcare organizations.
Yes. RCM products integrated with EHR/EMR systems can provide patient details. This feature enables providers to access patient data easily at one centralized location. Integration with electronic health records reduces the burden of manual entry. With this feature, our RCM platform enables providers to focus more on delivering quality care. This feature also reduces the chances of human errors and inaccuracies in medical records.
For tracking financial performance, our RCM software includes user-defined reports, KPIs, analytics, and dashboards for in-depth insights. Comparative analytics help organizations benchmark their revenue cycle performance against peers, driving performance enhancements. Real-time insights, derived from claims and remittance data, enable immediate action. Dashboards and reports pinpoint areas for improvement throughout the revenue cycle process, such as coding, billing, and receiving, facilitating more effective financial management.
Robotic process automation handles repetitive tasks like data entry, eligibility verification, and claims submission, reducing errors and enhancing efficiency through our product. Real-time eligibility verification recovers patient insurance coverage details. Automated billing and claims management processes ensure timely and accurate submissions, while automated payment posting reduces manual data entry errors, enhancing accuracy throughout the revenue cycle management.
Our RCM technology uses various automation tools to effectively manage denials and claim rejections which facilitate revenue recovery. Denial management automation investigates denial root causes, speeds up resubmissions, and minimizes denied claims. RPA streamlines data entry, eligibility verification, and claims submission, reducing errors and enhancing efficiency. Real-time eligibility verification recovers patient insurance coverage details. Automated billing and claims management ensures accurate and prompt claim submissions and real-time tracking, contributing to efficient revenue recovery.
Our system facilitates transparent billing and enhances patient understanding of financial responsibility, reducing inquiries. Patient portals enable bill viewing, payments, and direct communication with healthcare providers. Real-time eligibility verification recovers insurance coverage details. Automated billing and claims management streamlines claim submissions and real-time tracking. Dashboards and reports pinpoint areas for improvement in the revenue cycle process, spanning coding, billing, and receiving, enhancing patient financial interactions and billing efficiency.
Our software automates administrative tasks like data entry, eligibility verification, and claims submission, minimizing errors and enhancing efficiency. Transparent billing reduces patient inquiries, while real-time eligibility verification streamlines insurance coverage details. Automated billing and claims management processes accelerate claim submissions and tracking. Comparative analytics helps in benchmarking performance against peers, identifying areas for improvement, and driving efficiency enhancements.
Our RCM product seamlessly integrates with EMRs to streamline billing and coding processes. Real-time eligibility verification ensures up-to-date insurance coverage details. Automated billing and claims management accelerates claim submissions and tracking. Patient portals facilitate bill viewing, payments, and communication with healthcare providers. Comparative analytics enable performance benchmarking and pinpointing areas for improvement.
We offer a wide range of customization options in the RCM software. Users can add or delete modules as necessary, enhancing software utility and managing costs. Integration with EMRs streamlines billing and coding. User-defined reports, KPIs, analytics, and dashboards are available for in-depth insights. Comparative analytics helps in benchmarking, identifying improvement areas, and enhancing performance.
Our software assists in patient eligibility verification and insurance claim accuracy through real-time eligibility verification, which recovers patient insurance coverage details. Automated billing and claims management speed up submissions. Transparent billing enhances patient understanding, reducing inquiries. Comparative analytics enable performance benchmarking, identifying improvement areas, and driving performance enhancements, collectively ensuring precise insurance claims and improved revenue cycle management while reducing patient billing inquiries.